Season 6 of The Big Unlock podcast captures a defining moment for healthcare. Across conversations with CIOs, CMIOs, CMOs, CAIOs, digital transformation leaders, and innovators, one message comes through clearly: artificial intelligence has moved beyond experimentation. In 2025, AI is no longer something healthcare organizations are “exploring,” it is becoming embedded into how care is delivered, how work gets done, and how health systems think about scale, sustainability, and growth.
Season 6 reveals a deeper transformation, leaders are rethinking workflows, workforce models, patient access, governance, and the economics of care, with AI acting as an accelerator rather than a silver bullet.
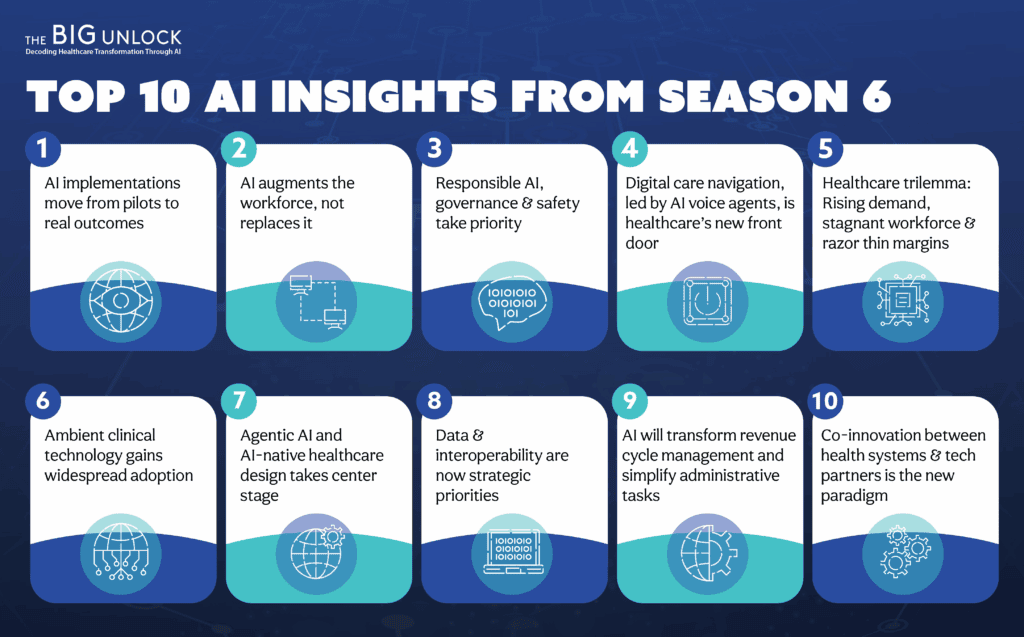
Here are the Top 10 trends discussed throughout the 2025 season, a reflection of what healthcare leaders are prioritizing today and where the industry is headed next.
AI Is Becoming Operational: Moving Beyond Pilots to Real Outcomes
One of the strongest signals from Season 6 is that AI has crossed the pilot phase. Health systems are no longer satisfied with proofs of concept; they are demanding measurable, operational impact.
Guests across the season described how AI is now embedded into day-to-day workflows, from clinical documentation and scheduling to capacity management and care coordination. These deployments are delivering tangible results: reduced clinician burnout, improved access, faster turnaround times, and more efficient use of limited resources.
What differentiates successful organizations is not the sophistication of the technology, but the discipline of implementation. Leaders emphasized that operational AI requires governance, workflow redesign, and ongoing measurement – not one-off experiments.
The message is clear: 2025 is the year AI became real for providers.
The Rise of Ambient Clinical Technology
Ambient clinical listening emerged as one of the most discussed and widely adopted technologies in Season 6. Rather than being framed as a documentation shortcut, ambient technology was described as a fundamental shift in how clinicians experience care delivery.
By capturing conversations in real time and generating structured clinical notes, ambient tools reduce after-hours documentation and allow clinicians to remain fully present with patients. The result is not only time savings, but also better clinician-patient relationships and improved note quality.
At the same time, guests were clear that success depends on thoughtful rollout. Training, trust, and change management are critical. When implemented responsibly, ambient technology is quickly becoming foundational to modern clinical practice.
The Shift to Agentic AI and AI-Native Healthcare Design
Season 6 marks a noticeable shift from generative AI that supports tasks to agentic AI that can take action. Leaders discussed AI agents that can handle referrals, manage prior authorization workflows, coordinate care tasks, and support operational decision-making.
This evolution signals a broader transformation toward AI-native healthcare design. Instead of layering AI on top of existing processes, organizations are beginning to redesign workflows around intelligent systems that operate within defined guardrails and escalate to humans when needed.
While still early, these discussions make it clear that agentic AI will play a critical role in scaling care delivery without proportionally increasing workforce size.
Workforce Augmentation: AI as a Partner, not a Replacement
Across Season 6, leaders were remarkably aligned on one point: AI is not about replacing clinicians, it is about enabling them.
Guests described how AI is taking on repetitive, administrative, and low-value tasks, allowing clinicians to focus on complex decision-making, patient relationships, and care quality. This shift is particularly important in an environment marked by workforce shortages and burnout.
However, adoption depends on trust. Clinicians need to understand how AI works, where its limits are, and how decisions are made. Season 6 reinforces that the future workforce will be defined by effective collaboration between humans and intelligent systems.
A recurring message: AI should free clinicians to practice at the top of their license.
Data Infrastructure & Interoperability Are Now Strategic Priorities
Another recurring theme is the realization that AI success is fundamentally a data problem. Without clean, connected, and interoperable data, even the most advanced models fail to deliver value.
Guests emphasized investments in cloud platforms, standardized data pipelines, and interoperability frameworks. Pediatric networks, population health initiatives, and enterprise AI strategies all pointed to the same conclusion: data infrastructure is no longer a back-office concern, it is core to clinical and operational strategy.
In 2025, data readiness is increasingly viewed as a prerequisite for innovation rather than a downstream technical task.
Data modernization is no longer an IT project, it is enterprise strategy.
The Importance of Responsible AI, Governance & Safety
As AI adoption accelerates, Season 6 makes it clear that governance has become a top priority. Leaders spoke openly about the risks of deploying AI without appropriate oversight, particularly in clinical and administrative decision-making.
Many organizations have established formal AI governance structures that include clinicians, technologists, compliance teams, and executive leadership. These groups are responsible for evaluating use cases, monitoring bias, ensuring safety, and setting boundaries for automation.
Rather than slowing progress, responsible AI practices are helping organizations scale with confidence and build trust among clinicians and patients alike.
The theme: Responsible innovation is not optional, it’s foundational to trust.
Digital Care Navigation Is Becoming the New Front Door
Several episodes highlighted a shift in how patients access and experience care. Digital care navigation platforms are increasingly serving as the “front door” to healthcare, guiding patients to the right care setting at the right time.
AI-powered navigation tools help reduce friction, improve access, and optimize system capacity. For health systems, they also play a critical role in managing demand, improving patient satisfaction, and supporting growth strategies.
Season 6 positions digital navigation not as a consumer add-on, but as essential infrastructure for modern healthcare delivery.
AI in Revenue Cycle and Administrative Simplification
While clinical use cases often dominate AI conversations, Season 6 repeatedly underscored the massive opportunity in administrative and revenue-cycle workflows.
Leaders discussed how AI can streamline prior authorizations, reduce denials, improve documentation accuracy, and automate routine administrative tasks. Given the scale of administrative costs in healthcare, even modest efficiency gains can have outsized financial impact.
These discussions reinforce that some of AI’s most immediate and sustainable value lies in simplifying the non-clinical work that burdens care teams and organizations.
This is one of the most financially meaningful areas for AI in 2025.
Co-Innovation Models Between Health Systems and Technology Partners
Another important trend is the rise of co-innovation models. Rather than buying off-the-shelf solutions, health systems are increasingly partnering with technology companies to build solutions together.
This approach allows tools to be shaped by real-world clinical workflows and operational constraints. It also accelerates adoption, as clinicians and leaders have a stake in the solution from the outset.
Season 6 shows that co-innovation is becoming a preferred path for developing scalable, relevant, and trusted digital solutions.
The “Healthcare Trilemma”: Rising Demand, Workforce Shortages & Margin Pressure
The final trend ties many of the season’s themes together. In the episode focused on solving healthcare’s trilemma, leaders articulated a structural challenge facing nearly every health system: rising patient demand, persistent workforce shortages, and increasing financial pressure.
The conversation emphasized that traditional growth models. hiring more staff or adding more facilities, are no longer sufficient. Instead, organizations must focus on disciplined prioritization, co-innovation, and AI-enabled orchestration of care.
This trend reinforces a central message of Season 6: AI is not just a tool for efficiency. It is becoming essential to healthcare’s long-term resilience and sustainability.
Looking Ahead: Setting the Stage for Healthcare’s AI-Driven Future in 2026
The conversations in Season 6 of The Big Unlock paint a clear picture of healthcare in 2025. AI is no longer peripheral. It is reshaping how care is delivered, how clinicians work, how patients access services, and how health systems remain viable in an increasingly complex environment.
The real “big unlock” is not adopting AI for its own sake, but using it to redesign healthcare around people, data, and intelligent systems – responsibly, thoughtfully, and at scale.
The “big unlock” for 2025 is not simply adopting AI tools.
It is redesigning healthcare around AI, moving from incremental change to structural transformation. Health systems that embrace these themes will shape the next decade of healthcare delivery.
