The senior living industry is undergoing a quiet revolution. What was once viewed primarily as housing for older adults is transforming into a holistic health and wellness ecosystem, where housing is just one part of the story. Michael Hughes, Chief Transformation and Innovation Officer at United Church Homes, is at the forefront of this change — driving initiatives that combine affordable housing, healthcare partnerships, advanced technology, and human-centered care models to better serve an aging population.
In a recent episode of The Big Unlock podcast, Mike shared his perspectives on where the industry is headed, the role of social determinants of health (SDOH), and why co-creation and prevention will define the next chapter of senior living. His message is clear: the future will be more connected, more personalized, and more prevention-driven than ever before.
United Church Homes operates more than 100 properties across 15 states and two tribal nations, encompassing affordable housing, life plan communities, skilled nursing, and independent living. But Mike believes the industry’s future isn’t about the physical buildings — it’s about integrating housing with wraparound services that help older adults remain healthier, happier, and more independent for longer. He states that, “The future of senior living is transitioning from housing providers to health and wellness providers with housing at its core.”
This shift requires a mindset change. Instead of focusing solely on residents who can relocate into communities, United Church Homes is building partnerships with CMS programs, managed care organizations, and local service providers to bring services directly to where people live.
Their decentralized, hub-and-spoke model allows the organization to support older adults who may never move into a senior living facility but still face challenges in managing health, safety, and daily living. For Mike, this approach is not just about expanding reach — it’s about meeting people where they are and creating sustainable models for the future.
One of United Church Homes’ most impactful innovations is its service coordination program in affordable housing communities. Funded through HUD, these coordinators assess residents’ social determinants of health — the non-clinical factors such as transportation, food security, financial stability, and home safety that account for roughly 70% of health outcomes.
The impact is measurable and remarkable. Out of 3,200 affordable housing residents with service coordination, only 50 moved into skilled nursing facilities and 110 experienced unplanned hospitalizations over a 15-month period. For a population often living with multiple chronic conditions, these numbers are exceptionally low.
Mike credits this success to a trust-based, relational care model. Coordinators do far more than connect residents to resources like Medicaid waivers or home health agencies — they also provide emotional support and guidance during health crises. He says, “Nobody takes their pills because they like how they taste. We build care plans around personal goals and motivations.” This focus on personal motivation — whether it’s wanting to keep a beloved pet, maintain a garden, or attend a local art exhibit — turns care into a collaborative process rather than a compliance exercise.
By unbundling service coordination as a standalone service, Mike sees potential to integrate it into managed care programs, employer wellness benefits, and long-term care insurance models — particularly for high-cost, high-need populations.
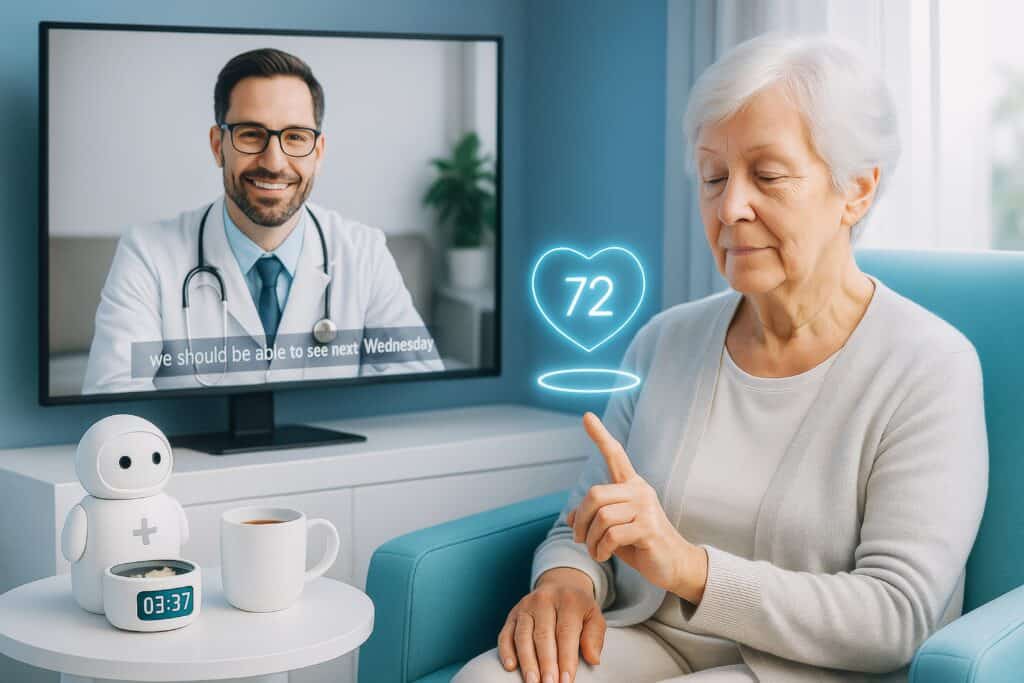
While technology is often positioned as the silver bullet for healthcare challenges, Mike approaches it with a clear focus on prevention and practicality. His innovation strategy prioritizes tools that generate actionable insights and measurable outcomes, rather than chasing every new gadget.
Machine learning currently tops his list, especially for analyzing the effectiveness of community referrals and identifying which services truly improve health outcomes. By combining clinical and non-clinical data — such as functional status, home safety, and caregiver availability — United Church Homes is building predictive models that can guide earlier interventions and strengthen value-based care partnerships.
Some of the most promising solutions are also the most cost-effective. For example, Mike is testing RFID tags in shoes to monitor mobility patterns, replacing more expensive and complex sensor systems. This approach aims to capture 60% of the data that drives 80% of the insights — at a fraction of the cost.
He also sees potential in agent-based AI for automating routine but time-consuming tasks, such as arranging transportation after a doctor’s appointment or processing prescription renewals. If done right, this could free human staff to focus on relationship-based care, where the greatest value lies.
For Mike, successful innovation in senior living starts with deep immersion in the environment you want to improve. That belief inspired United Church Homes’ Entrepreneur-in-Residence program.
Participants in this program live in a senior living community for two weeks. The first week is spent shadowing staff to understand operational realities; the second is a “choose your own adventure,” where participants adopt the persona of a new resident and experience daily life firsthand.
This immersive approach helps innovators fall in love with the problems before proposing solutions. It reveals nuances of resident experience, staff workflows, and organizational culture that would be missed in a traditional consulting or product design process. Mike says, “Unless you co-create with the people you aim to serve, you have no load around your system.”
The program has already sparked collaborations and produced solutions that are better aligned with resident needs, easier to implement, and more sustainable. Mike hopes to see other senior living providers replicate this model as a best practice for human-centered innovation.
Looking ahead, Mike envisions a more distributed model of senior care — one that extends far beyond the walls of any single facility. This future will be supported by technology, community partnerships, and purpose-driven engagement.
One concept gaining traction is social prescribing — where healthcare providers “prescribe” community-based activities such as nature walks, museum visits, or volunteer work to combat loneliness, boost mental health, and encourage physical activity. Countries like the UK and Canada have embraced this approach, and Mike believes it could play a major role in U.S. aging services as well.
At the core of his vision is the idea that purpose is as important as care in later life. Whether it’s spending time with grandchildren, tending a garden, or pursuing a creative hobby, these motivations should anchor care plans and guide service delivery.
Mike also emphasizes the need to remove daily life frictions — from home maintenance challenges to transportation gaps — so older adults can maintain independence and dignity. This, he says, is where innovation should focus its energy: creating systems and services that empower older adults to live abundantly in the place they choose.
Recent Blog Posts
Stay informed on the latest in digital health innovation and digital transformation