Insights from Dr. Chris Gallagher on The Big Unlock Podcast
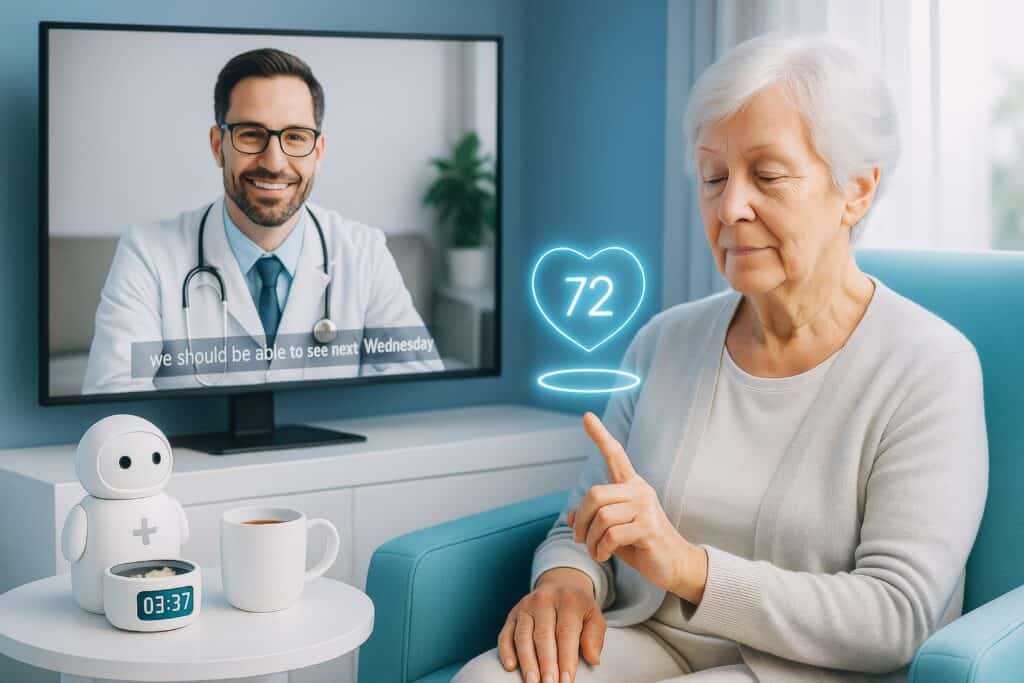
Virtual care is no longer an experiment. It is becoming a core part of modern healthcare delivery. In a recent episode of The Big Unlock podcast, Dr. Chris Gallagher, Founder and Chief Strategy Officer at Access TeleCare, discussed the shift toward hybrid care models, how virtual care, tele-ICUs, and AI are reshaping physician distribution, hospital operations, and the patient experience, especially for underserved communities.
Chris’ story is both personal and systemic, rooted in early exposure to underserved communities, years before telehealth entered the mainstream. His experience provides a real-world blueprint for how virtual care models can solve persistent physician shortages, expand specialty care, and create safer, more efficient patient experiences.
From Rural Weekends to Virtual ICU Pioneer
Chris’s journey into telehealth began as a cardiology trainee spending weekends serving rural communities around Dallas, where he saw the same level of disease complexity as in major academic medical centers, often worse because conditions went undiagnosed for years. That experience convinced him that geography should not determine the quality of care, and it sparked a career-long focus on high-acuity, underserved patients.
When recruitment of on-site specialists failed, he and his colleagues turned to telemedicine, eventually building the first virtual ICU in Texas in 2013. And on its third night, the program helped save a life and cemented his conviction that virtual care needed to be his life’s work.
Overcoming Early Resistance to Telemedicine
Launching tele-ICU a decade before COVID meant pushing against skepticism from clinicians who questioned whether virtual models were “real medicine”. To win trust, Chris’s team limited their initial efforts to a single ICU for a year, proving safety, outcomes, and ROI before scaling.
He describes the long stretch from 2014–2016 as mostly educating health systems, with a turning point around 2018 when leaders needed less explanation and more implementation. Then the pandemic accelerated acceptance by at least a decade and normalized virtual care as a core modality.
Making Technology “Fisher-Price Easy”
One of Chris’s central themes is that technology must be radically simple if clinicians are going to use it in the chaos of real-world care. Early on, a virtual encounter required 27 steps for the physician and 13 for the nurse, which created friction and slowed adoption.
His team adopted a design mantra – “Fisher-Price easy,” and relentlessly removed steps until clinicians could connect with a patient almost as easily as pressing a single button. As the user experience improved, encounters increased and adoption became self-sustaining, a pattern he believes will repeat with AI if solutions are intuitive and reliable.
Solving Physician Distribution, Not Just Rural Access
While the origin story was rural underserved care, Chris emphasizes that the main telehealth use case has shifted dramatically. In just three years, Access TeleCare moved from serving 70% rural and 30% urban patients to the reverse – 70% urban and 30% rural.
Today, virtual programs are as likely to support large city hospitals as small rural facilities, especially where there is only one on-site specialist who can never take a day off without leaving gaps in coverage. Telehealth becomes a “programmatic envelope of care,” adding fractional virtual FTEs around local clinicians so hospitals can achieve 24/7 coverage without burning out the in-person team.
Virtual Coverage as a New Staffing Model
Chris describes a new staffing paradigm where hospitals no longer try to fully staff every specialty on-site around the clock. Instead, they:
- Use virtual clinicians to cover nights, weekends, and low-volume periods.
- Allow scarce specialists (like infectious disease or intensivists) to focus on clinic or procedures while telehealth handles inpatient consults.
Because 66% of hospital time is nights and weekends, covering everything purely in person is either impossibly expensive or unsustainable for clinicians, whereas virtual care can be scaled “dose-dependently,” used only as much as needed, without idle capacity.
AI, Automation, and The Digital Back Office
For Chris, AI is not abstract; it is already embedded in practical workflows. His organization is piloting AI in back-office areas such as revenue cycle and operational automations, as well as in clinical routing and scheduling to support nearly 800 physicians and nurse practitioners.
Over 50% of consults now flow through digital automation rather than phone calls, with EMR-integrated workflows that let hospitals trigger a consult at the push of a button and route it directly to the right specialist’s mobile app. AI will make this routing smarter and faster, enabling his team to reach the bedside up to 20% sooner, crucial for emergencies like acute stroke or cardiac arrest.
Voice Agents and The Next Wave Of AI
Chris is optimistic about voice agents as a natural evolution in AI-enabled care. His team is actively running pilots with multiple vendors to determine which tools best fit their physicians and advanced practitioners, focusing on both efficiency and experience.
Most current use cases they are exploring sit behind the scenes – supporting revenue cycle, documentation, and operational workflows, rather than replacing the human interaction at the bedside. The goal is not to remove clinicians from the loop but to free them from administrative burden so they can spend more time in clinical decision-making and patient communication.
Redefining The Digital Front Door For Acute Care
Unlike many digital health companies that focus on at-home consumers, Access TeleCare’s “digital front door” starts inside hospitals. All of their patients are in emergency departments, ICUs, inpatient floors, or clinics, and many encounters are unscheduled, triggered by sudden changes in condition.
Instead of patients booking online, hospitals initiate virtual consults directly from Epic or Cerner, routing requests into a centralized platform that balances workload among specialists in seconds. This model turns telehealth into an invisible backbone of acute care, embedded in hospital operations rather than acting as an external service layer.
Making Virtual Care Feel Like In-Person Medicine
To win clinician and patient trust, Chris insists that virtual encounters must feel as close as possible to traditional bedside care. Each hospital is equipped with a six-foot telemedicine cart featuring a large display, high-resolution zoom camera, and digital stethoscope so remote physicians can read monitors, view ventilator settings, and perform detailed physical exams.
There is always a “patient presenter” in the room – usually a nurse, medical assistant, or ER physician – to provide hands-on support and carry out parts of the exam, while the remote physician documents, orders, and manages treatment within the hospital’s EMR as any on-site clinician would.
Health Equity, Local Care, And Cost Savings
A major impact of these programs is on equity and local access. Around 82% of the patients Access TeleCare serves are underserved, including uninsured, Medicaid, and elderly populations who would otherwise face delayed or fragmented care.
By bringing specialists to the bedside virtually, hospitals avoid costly transfers that can add about $5,000 per episode and, in the case of helicopter transports, tens of thousands of dollars more—costs that ripple through families and communities. For roughly the price of a $200 telemedicine consult, hospitals can keep patients in their home communities, close to their support systems, while still delivering high-quality specialty care.
Toward A Virtual-First, Hybrid Future
Strategically, Chris sees health systems moving toward “virtual-first” models in many non-procedural specialties. In this vision, every patient is guaranteed baseline access to specialty care via virtual providers, and in-person clinicians are layered on top for procedures and high-volume needs.
He argues that traditional physician staffing models, largely unchanged for a century, are no longer tenable in an era of workforce shortages and rising demand. Virtual care provides the flexibility to dial resources up or down, matching supply to demand without overworking clinicians or paying for idle capacity.
A Turning Point for Medicine
Chris places AI and virtual care alongside antibiotics and modern surgical techniques as potential turning points in medical history. COVID, he notes, didn’t just accelerate telehealth adoption—it fundamentally lowered healthcare’s resistance to change and opened the door for broader digital transformation.
He is bullish that AI will significantly enhance organizational efficiency, improve the physician experience, and ultimately elevate patient care, provided that governance, privacy, and safety guardrails are in place. For Chris Gallagher, the future of healthcare is hybrid, AI-enabled, and deeply human—using technology not to replace clinicians, but to extend their reach to every patient who needs them, wherever they are.
