Coronavirus conversations
Coronavirus conversations
Dr. Ram Raju, SVP and Community Health Investment Officer at Northwell Health
"We need to figure out how to make the shift from face-to-face medicine to virtual medicine"
 Hosted by Paddy Padmanabhan
Hosted by Paddy Padmanabhan 
Share
In this episode, Dr. Ram Raju discusses how the global COVID-19 pandemic has impacted Northwell Health and how in future healthcare delivery systems will change in response to the crisis.
Northwell Health is one of the largest health systems in New York and has been a telemedicine leader for several years. Dr. Raju believes that healthcare systems will need to evolve and change their workflow as more and more people will be seeking care through virtual technologies. Primary care will leverage technology to shift face-to-face medicine to virtual medicine, while specialty care will stay in the hospitals.
Dr. Raju also believes that storing data in the EHRs and EMRs is going to be very different in the future with more data in video clips than text notes.
Dr. Ram Raju, SVP and Community Health Investment Officer at Northwell Health in conversation with Paddy Padmanabhan, CEO of Damo Consulting on the Big Unlock Podcast – “We need to figure out how to make the shift from face-to-face medicine to virtual medicine”
PP: Welcome back to my podcast. This is Paddy and it is my great privilege to introduce my special guest today, Dr. Ram Raju of Northwell Medicine in New York. Dr. Raju, thank you so much for setting aside some time and welcome to the show. New York has been at the center of the COVID-19 pandemic. Can you share a little bit about what the experience has been at Northwell and how it is impacted Northwell and share a little bit about your COVID-19 response efforts?
RR: This is something which none of us ever prepared for, even dreamt about. Northwell, as well as the other healthcare delivery systems in New York City, has really raised up to the challenge and especially the providers and the frontline workers have done a fantastic job of managing the flow of the patients, testing them, treating them, and able to stay with the patients and putting themselves at great risk. The health system has done a remarkable job of trying to save as many people as they could. So, this has been a story of the greatest success. We should be in this country, which really had such a devastating epidemic with a tremendous amount of sacrifice on the part of the people to get this done. Now we see a diminution of the number of patients who are coming to our EDs with the virus syndromes, as well as to the number of people who are in the ICU and the number of people who are on the ventilator. All of them are showing a very, very good downward trend. So, it looks like we are probably behind the apex of the curve, but this also has to do a lot with what the government has done and also the discipline of the New Yorkers in practicing very, very strict social distancing, which has helped us a lot.
PP: Thank you for providing us with that background. I hope for the sake of New Yorkers and for everyone else across the country and the world, that we put this behind us as soon as possible. The healthcare impact and the immediate need of having to identify and treat those that are infected with COVID-19 is one part, there is obviously a significant financial impact to the broader economy as a whole because of the shelter at home and the health systems in particular as a result of the pandemic. I know that the federal government has done its best to help through CARES Act to set aside some money at 100 billion to help hospitals deal with additional costs. Is that making a difference? What is the outlook for hospitals and health systems in financial terms in this coming year?
RR: Healthcare systems in the country have always been on a very thin margin and they do not have much in savings to fall back on. That is true for most of the healthcare delivery systems of the country and New York City is no exception. This has produced a tremendous amount of financial burden on healthcare delivery systems. And the health of the federal government is definitely very much appreciated and very much welcome. And it is also extremely important to keep the healthcare delivery system going in New York City. But the long-term economic issues will be devastating because we have not seen what the long term outlook looks like even after the pandemic is well past us. We will take a long point of time, the economy to gear up to the level it has been there before the pandemic, as well as the confidence of the people able to go back to those restaurants in New York City, those tourist spots, those games, and all those things will take a long time for the New Yorkers and all across the country to get back to the way things were. People have started talking about the new normal after this pandemic. We are going to see a different way of people reacting to it which is unpredictable. I think a large portion of the economic recovery depends on individual behavior. How much confidence they will have in going back to doing things they have done before this without batting an eyelash.
PP: That’s very well-said. Healthcare went overnight to a virtual care model. I imagine like with other health systems across the country, Northwell too accelerated significantly in terms of its journey towards telehealth mode of delivering care. Could you talk a little bit about what some of those big changes in virtualizing your care delivery?
RR: Northwell has been a leader in telemedicine for the last five or six years. And we have used the telemedicine capabilities across our system very effectively in teleradiology, telepsychiatry was a major component of it. And also, our transitional care workers use telemedicine to a great extent to follow up on the patients at high risk and also be used extensively on our readmissions task force and making sure that the people are really taking care of. Having said that, it accelerated tremendously after our experience with the coronavirus. There was a little bit reluctance on the part of the patients adhere to this telemedicine concept. But this pandemic opened eyes and it made it more normal for the patient perspective to be able to get on a telemedicine call and able to chat with the patient. So, in the new normal there will be less reluctance. There is a huge cultural change that has happened. And people will be getting more and more care and consultations through virtual technology to a great extent. So, we need to get it out, get this up. That simply means that most of the healthcare delivery systems in this country have got to really change the workflow issues. There may not be as many patients ever coming to the clinics. And there may be a good number of people probably be seeking care and getting advice through virtual technology. So that simply has got different kinds of processes we need to evolve. We need more people who are having the telemedicine concept. That means we need more hardware, more software, and more situation room kind of things where we are able to guide the patient through the system effortlessly and with minimal delay. But at the same time, on the flip side, the real estate value of having these large clinics, there are large waiting rooms and all those things need to be rethought because there may not be as many people coming through who occupy those waiting rooms in the large clinics which some of the hospitals have built, very recently, to accommodate more flow. We need to really figure out how do we make the shift from face-to-face medicine to a virtual medicine and all the implications with come that. We need to gear up certain areas of our support system to accommodate high demand on the virtual and our doctor’s visit. And we may have to shut down some other areas of the healthcare delivery system which will not be needed as much in the new normal after the coronavirus.
PP: What does that mean for the healthcare sectors? Are you anticipating that there will be more M&A and consolidation? And to a point, inevitably some hospitals just closing. And what does it mean for healthcare consumers in general, especially for vulnerable populations or rural populations?
RR: What will happen is that the places which cannot be done virtually like an operation, or delivering a baby, or some of those things who need to be done in a hospital and are basically a face to face functions. Apart from that the organizations which has a huge reach of telemedicine capacity will probably eat up into the market of the people with the telemedicine were able to attach to the doctors. In other words, if I have an opportunity to attach myself to a hospital A where I was getting my face-to-face care, now I can attach myself with the same ease to another hospital. Hospital B which is like a large teaching hospital. I would prefer to go to hospital B because now the distance does not matter. The geography does not matter anymore. In the past, the geography, the distance mattered where I needed to go to the nearest place. I don’t want to travel like in all 50 miles to go and see a doctor. But now that has changed. So, there will be a tremendous re-shifting of the healthcare delivery system in this country. You will see the hospitals, which are basically doing mostly straightforward medical patients, will probably have a very tough time keeping their doors open. But a hospital might have done, as some specialists like in orthopedic surgery are a neurosurgeon, a spine surgery that cannot be done through telemedicine, though naturally, they will be more in demand. So, we will probably shift from primary care to virtual technology and specialty care will probably sit in the hospitals. And the hospitals need to figure out how can they shed their primary capacity real estate and acquire more real estate on the specialty.
PP: Talking about even the primary care shift in the telemedicine, there are sections of the population, vulnerable, low income, rural, and many others that are still not necessarily placed to receive care for telemedicine modality as a large urban environment that I’m kind of pointing out. There are two extremes here. But do you think that vulnerable populations may not benefit as much from telemedicine as maybe other parts of the population?
RR: You are absolutely correct. That is the point I was making in my last webcast. The problem is this is a group of people or I call them socially vulnerable populations, which has been my main focus for the last 19 years and trying to figure out how can we create health equity, social equity, and social justice for the population so that they can have a level playing field. And that has been a major concern. So there are people who do not have either the literacy level, the knowledge level to able to get this technology and the able to utilize the technology or the inability to access to a computer or a fast internet, which will make those virtual care easier. And then the language issues which come along. I am worried that it will create more health care disparities for this socially vulnerable population. This is the population we call social determinants of health. The population which lives in the food deserts, live in their transportation desert, population who are living in a publicly unsafe. These are people who live in a public housing with a large lead poisoning effect, all those stuffs which they suffer. Now, the fact of the matter, they tell you this healthcare is also shifting to a technology which they are either not capable of utilizing and or they don’t have the technology to get it done will probably be left behind. That has been my major, major concern. But the problem with that is it is apathy. I believe that there will be a further division of the healthcare delivery system in this country from their ability to pay issue will be hospitals which purely cater to the people who are socially disadvantaged, like public hospital systems in the country. And then there are hospitals which are basically catered to the people was got good insurance. So, the two-tiered healthcare delivery system will get further divided. There will be a bigger division and a bigger gulf between their haves and have nots in this country. We will have no further damage; I think the vulnerable population. So I’m very worried about that because the problem with that is the hospitals, which are really trying to stay at the cutting edge of this will probably invest more time and energy on the telemedicine, teleradiology, and telepsychiatry they’re using virtual care will probably think in better investing than opening up the face-to-face encounter, which will probably be widely utilized mostly by socially disadvantaged people. Another name for them is people who are poor, and they can’t afford, and they have no insurance and they are very underinsured people. So, this is a problem which will happen. There will be another shift of the values in this and the question comes in, how do you protect them and that is a bigger question to ask.
PP: There is a lot of food for thought there Dr. Raju. Talking about the technology itself. So, in my podcast, I mostly talk about digital technologies and digital transformation itself for health systems. Now we have obviously seen telehealth kind of take-off and all the visit visitor numbers are going through the roof because of COVID-19. What do you see that health systems across the country are now going to be compelled to accelerate their digital transformation and accelerate their investments in technology to transform the way they deliver care, not just in virtual visits, but a whole range of other things, remote patient monitoring, and AI-led diagnosis and treatment, what is your view on that?
RR: Absolutely, we have learned finally to break the barrier, the cultural barrier of some people believing that they are getting a business done through virtual technologies, somehow inferior to a face-to-face encounter, that is broken. So that means that flood gates are going to open. People are not reluctant anymore to seek care and they’re happy with the care they get through a virtual technology. This is completely going to change the way and most of the hospitals are going to raise towards creating the digital platforms and digital technology in acquiring or contracting that out to take care of the patients. It has really changed the way we do that. And also the way they function, one of the things the hospital systems are seeing like any business system in the country that a good portion of the hospital employees can do not need to be in the hospital or in the corporate headquarters to provide care. They can stay at home and work remotely. And that has created other issues, there will be about one third of the hospitals, a large workforce, maybe working remotely. So that also creates another, both on the employee’s side, how do we manage them when they work remotely, and also from the patient perspective, how can we use digital technology to reach more patients in a much more effective way. All those things are going to make the hospital go in the next few years absolutely a race towards the technology, a race towards the digital platforms all the things that they need to do. Whether it is caregiving or remotely monitoring all those things are going to change your answer. So, there’ll be less of a footprint of the hospital and the footprint will be more by the digital technology, which extends its influence over a larger footprint than they ever imagined in the past.
PP: At the same time, we also must talk about the existing technologies and how we leverage those technologies to integrate them into the future state. So, I’m talking about EHR systems. There’s been a lot of talk about 35 billion, 40 billion in taxpayer money over 10 years. And of course, that is the single biggest digital transformation that has happened in healthcare over the last 10 years, just the digitization of patient records and clearing electronic workflows and so on. Now, some of the deficiencies are the shortcomings of electronic health record systems have been coming up. One of the biggest ones has been interoperability. We saw the final interoperability ruling go through earlier this year. Hopefully, the data flow among and within EHR systems for delivering care and having the access to the data at the point of care is going to get better. What are your thoughts on the final ruling and what improvements in care do you think that is going to result in as a result of the implementation of the final rule?
RR: Even before we talk about the final ruling, we need to think about what is in the EHR or EMR might look like in the future. Yeah, we are moving into the virtual care on telemedicine. The handwritten notes or the typewritten notes are gone. We will be storing the patient’s information and their visits through videos into their EMRs because no one is going to go back and write anything or type anything into it. It’s basically their EMR in the future will be, all of them are basically the video clips of meeting of the patient talking to them. So, the EHR will probably have less typing or less information. And then the video clips, that is what will probably happen over time. That means the interoperability, which has worked so hard to create and connect the various aspects of it will probably take a different turn. And, how do we store the video chats, which are coming from various places, eventually people will need to open the video chat into their smartphone, which has got different technology? People are going to use not just the computer; they want to use smartphone technology to talk to a doctor on their phone like they do FaceTime today. So, the question will be, how will you then we need to have a special way, because those conversations are not necessarily encrypted at the level. We have the documentation and the present time. The final rule is not going to be the final, final rule. It is going to be something very different in the future. So how do we do this, who gets information, who gets to see it? How do you play it back if you need to find that out? The components of the EMR will probably be going to change tremendously. How we store the data in the EMR is going to be very different in the future than it is today. So, we are still trying to make some amendments to strengthening the various rules and trying to get information organized and synchronized across away by all these rulings. Some of them will become moot point eventually because you will not be storing any more documentation in this story, mostly clips.
PP: That is such an interesting perspective. I’ve never heard anyone say that patient medical information in the future is going to be stored more as a video than as text. That is a fundamental paradigm shift in how we look at patient medical information. If that is the case, it needs interoperability and it needs for even being able to access the data in the form it is going to be available in places where it changes dramatically. That is so interesting. What do you see as a path for a return to normalcy and health care operations for the rest of the year?
RR: First of all, there will be new normal. We need to get used to that. There is no real way of doing things. Things are going to change tremendously and it’s going to be different. So, the new normalcy going to be in the future is not going to be in a year. We may open the shops; we may open the hospitals. We may be trying to go back to the way things were which will never be the way things were. Having said that, we are trying to get back to how the life was before it completely closed the economy and the communities and societies in our country. So, as we reopen it, we believe that it will go back to the way it was, but it will not be, it will be completely different. And you will learn as you go along. You will change your habits to great extent. We will probably do things very differently than we’ve done before. So, the economy has got to change with that idea. It’s like, I do not know that we’ll be sitting in a movie theater next to each other and feel comfortable watching the movie or watching the show. I am not sure it will be a stay in our sitting packed up in there in the Yankee Stadium and watch the game. So, all those things are going to change. So, the new normal will be very different. It is going to be, a lot more will be on the virtual level. Maybe there are more people watching those games and more movies on the on the streaming services as opposed to doing that. In fact, starting in a couple of one, one particular group has actually started releasing movies, not in the movie theaters, but streaming directly to the patient. They can actually go and buy the movie ticket and get it streamed into their home. That is a big thing. What will happen to the restaurants? Do we have to wait outside waiting for the restaurants? The normal, as you know, will be very different. This is very difficult to predict because we don’t know what it looks like, how much of tolerance and how much of confidence we will have is something which we do not know what I love. We’ll get better quickly and come back normal on it. Maybe it’ll be a change in life for a long time.
PP: My travel has come down to zero in the last couple of months and I have been a heavy traveler for decades and decades, and I just cannot imagine this. Someone told me this is like a 9/11 moment for healthcare care and more reason why travelers are not going to be the same again. Getting on a plane, sitting next to another anyway, just like you’re talking about Yankee Stadium or a Broadway show, life has got to change as well, among many, many other things. It’s going to be an interesting era, for sure.
RR: Yes, absolutely. That simply means it depends on the fact is how quickly the Broadway or the airlines trying to reorganize themselves and reconfigure the seats? It is going to be something we have to see. Maybe we will have less number of people traveling or more people willing to pay more money or people will be traveling more by car than by plane. So, there is going to be a big shift in transportation would not be in this country really quickly.
PP: Dr. Raju, it’s been such a pleasure speaking with you. Thank you so much for setting aside time and I look forward to staying in touch.
We hope you enjoyed this podcast. Subscribe to our podcast series at www.thebigunlock.com and write to us at info@thebigunlock.com
Disclaimer: This Q&A has been derived from the podcast transcript and has been edited for readability and clarity.
About our guest
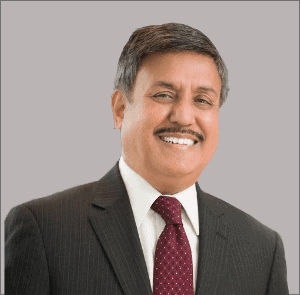
Ram Raju, MD, combines his executive leadership experience in healthcare with a deep commitment to achieving social equity to improve the health of communities in need. As the Senior Vice President and Community Health Investment Officer, he evaluates the needs of Northwell’s most-vulnerable communities and provides solutions for them by collaborating with community-based organizations. He is responsible for promoting, sustaining, and advancing an environment that supports equity and diversity, and helping the health system eliminate health disparities.
Prior to Northwell, Dr. Raju served as president and CEO of NYC Health + Hospitals from January 2014-November 2016. NYC Health + Hospitals has 42,000 employees, 11 acute-care hospitals, five nursing homes, six diagnostic and treatment centers, more than 70 community-based health centers, a large home care agency and one of the region’s largest providers of government-sponsored health insurance, MetroPlus Health Plan.
Dr. Raju also served as CEO for the Cook County Health and Hospitals System in Chicago, the nation’s third-largest public health system, where he improved cash flow by more than $100 million and changed the system’s financial health during his tenure from 2011-2014. His medical career began at Lutheran Medical Center in Brooklyn and he later served as Chief Operating Officer and Medical Director at NYC Health + Hospitals’ Coney Island Hospital. In 2006, Dr. Raju became the HHC Chief Medical Officer, Corporate Chief Operating Officer and Executive Vice President. Under his leadership, HHC continued to improve quality, patient safety, and health care data transparency.
Dr. Raju served as Vice-Chair of the Greater New York Hospital Association and currently sits on the boards of numerous cities, state, and national health care organizations, including the American Hospital Association, the New York Academy of Medicine and the Asian Health Care Leaders Association. Among his numerous awards and accolades, Dr. Raju was selected to Modern Healthcare’s “100 Most-Influential People in Healthcare.” Modern Healthcare also named him one of the “Top 25 Minority Executives in Healthcare” and one of the “50 Most-Influential Physician Executives in Healthcare.” In 2013, he was named a Business Leader of Color by Chicago United.
Dr. Raju earned a medical diploma and Master of Surgery from Madras Medical College in India. He underwent further training in England, where he was elected as a Fellow of the Royal College of Surgeons. He later received an MBA from the University of Tennessee and CPE from the American College of Physician Executives.
Recent Episodes
About the host
Paddy is the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy is also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He is the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He is widely published and has a by-lined column in CIO Magazine and other respected industry publications.
Connect