Season 3: Episode #105
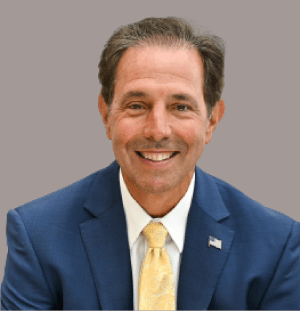
Podcast with Richard Ashworth, President and CEO, Tivity Health
"Digital health technology is helping people to engage in a healthier lifestyle"
 Hosted by Paddy Padmanabhan
Hosted by Paddy Padmanabhan 
Share
In this podcast, Richard Ashworth, President and CEO of Tivity Health, discusses why senior fitness is an important space and brimming with opportunities waiting to be capitalized. Tivity Health leverages core healthcare capabilities to deliver market-leading fitness, nutrition, and social engagement programs that improve health and lower healthcare costs.
In the episode, Ashworth talks about two significant macro trends in healthcare: the shift to digital health solutions and growth in Medicare Advantage. He further acknowledges how seniors have enthusiastically adopted technology but maintains that the future of healthcare is hybrid, i.e., a combination of digital and in-person care.
Healthcare is mission-driven and offers ample innovation opportunities in digital health, data, mental health, senior living, and home-based care. He advises youngsters to pick a job to make a difference, leverage opportunities, and continue to innovate and learn. Take a listen.
Show Notes |
||||
| 00:38 | About Tivity health and how you came into the role? | |||
| 03:42 | What are the macro trends you see playing out in healthcare as we head into 2022? How will they impact or influence your business? | |||
| 07:49 | Who are your consumers and who is paying for the services -- the health plans, the employers, the individual subscribers, all of them? | |||
| 12:10 | After the pandemic, telehealth kind of took off like a rocket. Wasn’t the case pre-Pandemic. Do you also see an analogous trend in your business? | |||
| 15:47 | Peloton and Apple Fitness come to mind first but where does your company fit in that milieu of online fitness? | |||
| 20:59 | Health systems are in a fee-for-service model and health insurance companies are trying to get everybody into more of an accountable care kind of a model. Do you see a tug of war between these two instincts? | |||
| 29:47 | What is your advice to the younger generation that is coming into the workplace today and is looking at healthcare as a career? | |||
About our guest

Richard Ashworth is the President and CEO of Tivity Health. He has spent his career focused on improving the health and well-being of others, with a passion for making a difference in the lives of customers and members. As a pharmacist, Ashworth has a keen understanding of the factors that influence health, including social determinants, adherence to treatment and a healthy lifestyle.
As President and CEO of Tivity Health since June 2020, Ashworth has brought financial stability and strategic focus to the business, prioritizing growth in the company’s core SilverSneakers offering and creating a digital-first strategy to drive further expansion. Previously, Ashworth facilitated the growth of Walgreens for nearly 30 years, transforming the company into a global leader in pharmacy and health and wellness. He most recently served as President, responsible for the leadership, development and management of all Walgreens operations.
Q. Tell us about Tivity Health and how you came into the role.
Richard: Tivity Health’s number one focus is on empowering people, communities, and partners and supporting them on their lives’ journeys. Our vision is healthier, happier, and more connected lives so we’re trying to help an aging population manage this in a couple of ways. One is through physical and virtual activities. So, we help people by giving them a gym membership and having them engage in physical, healthy behavior. We enable engagement and help people have social connectedness as well as mental enrichment. At Tivity Health, we also have a couple of other businesses like an integrated health service that has Chiropractic Care, Physical Therapy, Occupational Therapy, Acupuncture, Acute Therapeutic Massage etc. Our premier brand, Silver Sneakers, is the nation’s leading fitness program for older adults. Then, there’s also prime fitness, which is a discounted access to thousands of fitness locations. This is undertaken in partnership with commercial plans and employers. There’s also Whole Health Living, which is an integrative kind of health management business.
I started working as a stock boy at Walgreens when I was in high school, and really fell in love with pharmacy. So, I became a pharmacist. I just loved the way pharmacists worked within the community. You could walk up to any drug store and talk to a pharmacist any time, and they’d always be there to help you. So, it wasn’t just about the medicine; it was more about the community, the relationships, the life, and I was drawn to that aspect. I was at Walgreens for 30 years and by the time I left there as President, I’d held a lot of roles — commercial, operational, Strategic, International etc. Then, I came to Tivity and I’ve been here for 18 months.
I’ve spent my whole career on the treatment side of healthcare so, by the time I got to the people, they were taking medicine, were overweight, and struggling with health. I really do have a personal passion for fitness and nutrition and actually for the elderly, so I was keen to reach a spot that helped me do that well. There’s no better place in all of healthcare to do that than here at Tivity Health.
Q. What a fascinating story! So, Richard, what are the macro trends you see playing out in healthcare? How will they impact or influence your business?
Richard: I think there are two significant trends. One is more toward digital health solutions which have obviously been accelerated through the pandemic but were growing before. Then the pandemic hit, and digital health just took off at a stratospheric growth rate. The second is the growth in Medicare Advantage.
On the digital front, the seniors have adopted virtual solutions more readily than what everyone expected. That’s enabled us at Tivity Health to drive our SilverSneakers platform to deliver services differently than before. In fact, a recently published HHS study showed a 63-fold increase in the use of telehealth under Medicare during the pandemic. If you think about seniors using telehealth for their regular healthcare, while it’s hard for them to get around and go into offices, into facilities, then, that is a massive increase in the adoption.
When during the lockdown, many of our fitness locations closed, we quickly pivoted to offer virtual lives with instructor classes. Today, we’ve had more than three and a half million visits to those classes. So, the enthusiasm and the appetite are clear. We also have a pretty robust research engineer and so end up having lots of conversations with our members. These indicate that 85% will continue to use digital offerings in addition to visiting physical locations or fitness centers. Over 60% will use technology for video calls and live streaming with their friends and families. Over half will use it for medical appointments and fitness classes.
This tells me there’s a coalescing of adoption of digital health. Our members can choose from thousands of virtual activities, each week.
We’ve logged more than 3.4 million of that but many of those members are first-time users of SilverSneakers — almost half – that implies that the barrier to entry into maybe working out or engaging in a healthier lifestyle – technology, virtual or digital – whatever the term — is really helping people get into it for the first time.
On the Medicare side, 10,000 people age every day. It’s a fantastic entitlement program to take care of our older population. By 2030, the number of beneficiaries enrolled in the program is supposed to hit 80 million people. So just the sheer numbers require us to think very differently about this population and their expectations will also shift. The Baby Boomers coming in today versus those coming in 10 years from now will need very different technical capabilities and they’ll likely live longer. Those that get older later, will probably want to age in place with their own community, friends, family activities, while maintaining an active lifestyle. All this will influence the kinds of programs and services that get offered to seniors in the health and wellness space.
Q. The pandemic has accelerated the shift towards digital health. So, who are your consumers? You mentioned Medicare beneficiaries for your SilverSneakers program but who’s paying for the services — the health plans, the employers, the individual subscribers, all of them? Do explain.
Richard: The number one way we deliver SilverSneakers is through a partnership with the nation’s leading Medicare Advantage plans. So, the funder of the program makes this available to the beneficiaries. There’s no out-of-pocket cost for the members, themselves, since they sign up for their chosen Medicare Advantage plan. If Silver Sneakers is part of that then, they access this at no cost to them. Membership into our virtual experiences include social engagement, mental enrichment, and virtual fitness programs. In that context, members also avail of a robust gym network of up to 20-23,000 gyms across the United States. So, we share a goal with the health plan and that’s why it works so well. Not only us, but many times, the members themselves and the plan, really care about providing physical fitness options for older adults.
What we also care about is the community that’s built around that. So, the result of engaging with SilverSneakers is better health outcomes, lower healthcare costs. A study with Avalere Health showed savings in total annual average health expenses, including lowered medical and pharmacy costs. So, if you’re a SilverSneakers member, that’s a nod to $4463 in healthcare costs, versus an average of $5303 if you’re not. It is a significant reduction. It’s how a healthier lifestyle positively impacts your overall costs – for instance, somebody who works out is probably healthier than somebody who doesn’t; somebody who eats poorly probably isn’t as healthy as someone who eats well. What we do at SilverSneakers is help people engage in that healthier behavior. Sometimes it’s about food, other times about physical health or even mental and social aspects. What we see in our population on a like-for-like basis is 40% fewer hospital stays, 18% fewer visits to the emergency room and when they do go to the hospital, they stay 1.4 days less than those that are not SilverSneakers members. Being able to demonstrate this connection is important.
One of the other value propositions of SilverSneakers on the health side is that we’re really good and our brand is well-loved and understood, which enables the acquisition and retention of members within the plan. We get leveraged in the communications coming from the plans, which members like and so, they engage with that plan more often and stay longer.
On the service side, we help raise the overall customer service scores that health plans get just by having the SilverSneakers experience in close proximity. In fact, our NPS score is 83 and our customer satisfaction score is 96. We work alongside the health plans to promote healthier activity and drive this fantastic service experience.
Q. The pandemic obviously has changed the way a lot of services are delivered — Take telehealth as example. That wasn’t being used widely pre-pandemic but during the pandemic, online engagements shot up. Was that something you were already beginning to do or something that you built and rolled-out as a consequence of the pandemic? Now, telehealth engagements are reducing a little. Do you also see an analogous trend in your business?
Richard: I wish I could say that we were really planning for this, had a robust strategy before, and we knew that digital was the new frontier for senior fitness! It wouldn’t be true. We were really focused on getting people out and about and when the pandemic hit, we had to quickly pivot to the digital. We weren’t sure if that would work. There were so many misnomers all over — seniors can’t engage in technology as well as younger folk etc. It just turned out to be untrue. They are a lot more savvy than one gives them credit for. They’re on Facebook streaming live with families all the time so they are getting comfortable on the technology side.
Now, I come from retail. We’d been building “buy online, pickup in-store” for 10 years and had that capability at Walgreens for a long time, but nobody used it. Now, it’s become “let’s buy online, get delivered at home.” Taco Bell does it, too. And the pandemic has just cemented that into the fabric of how consumers operate. So, are we seeing that in our business? Yes. Do I see this as the future? I think it’s typical consumer behavior – there’ll be high demand and then a retraction and then, it’ll repeat quite like the rubber band. Peloton is seeing this, and others are seeing us.
For us, the future for SilverSneakers or for physical fitness is not 100% digital, and not physical or vice versa. It’ll be a hybrid world. I come from a consumer world, my mind is always consumer-oriented, so you just have to give consumers the choice and the experiences that they desire. Those desires will wax and wane so, today will not be important in three- or four-years’ time. As businesses, we must expand and retract alongside. The future then, is physical and digital.
I’ll share a quick example. In a letter from one of our members, she said she liked being at the YMCA though she also visited a 24-hour gym — that’s possible under our program so it’s a cool value proposition. Given how it rained one of those days, she as 73 years old didn’t want to drive but was keen on getting her workout. So, she attended our Zumba class with Sherilyn, one of our popular national trainers. We gave her an offering that she incorporated into the fabric of her life in a way that worked for her. And yet, we still had this other experience, if she wanted that. That’s a perfect instance of what we built here and why it’s applicable for her.
Q. The hybrid model is on everyone’s plans going forward. Peloton and Apple Fitness come to mind first but where does your company fit in that milieu of online fitness?
Richard: I love Apple Fitness and use it all the time at home. We’re all in the living room doing it together. So that’s a cool experience. I don’t view that as competitive but as additive.
If some of our members want to do that, that’s fantastic though it’s important that we adopt scientific ways in having the elderly work out. The reason I don’t really see Peloton as a competitor is for most of our members, I don’t want them up on a bike off the ground. There’s more of a risk for fall and if we have hip fractures then, that is detrimental to their health outcomes, in totality. So, we are very proprietary and clinical about how we do workouts.
We know what orthostatic hypotension is or how many times you should be getting on the floor and back up in a 10-15 minute period. We understand flexibility and mobility changes over time and the rigidity of tendons or how to exercise them. The audiences for those other companies are very different than what we’re talking about. What we try and do is deliver a best-in-class experience that has measurable value for the health plan. Fitness is so competitive when you go to YouTube and watch anything you want. But it may not be safe for some or for their condition or for where they’re at.
The other thing for us is we are live now and we have a full on-demand library to send everybody else. Some people like that and with our live sessions we highlight the community aspect and value that social connection. In Julia Hunt’s aging study, she found that if you wanted to live long, you needed to see the factors determining this – they could be your DNA, where you lived or even how many friends you had. When all the data and samples were considered, the number one conclusion was — people that had many friends lived longer. So, there is an inherent social community — evidence for us — that we must participate in.
On the competition front, our number one competitor are our members. You may like Apple Fitness, but there are days you’re in bed and you know you need to go workout but the biggest enemy preventing that is you. It’s not the access to the computer or to Apple. That’s who I see as the real competitor. We have 8-9-10% of our people work out regularly and I’d want that to be 80% but how do I get the remaining 70% to come? It’s not about giving them more gyms or a better virtual-online experience. It’s the intrinsic motivation. We do have traditional competitors, though and it’s worrying what everybody can do with our members because I’d like to ensure we’re here for them. That’s the way I see it.
Q. In the world of technology, the biggest competitor is usually a “do nothing.” Healthcare is driven by reimbursements or a fee-for-service model. The health insurance companies try to ensure an accountable-for-care model. Those in wellness and preventive care, your space, are into keeping people out of hospitals. Do you see a tug of war between these two instincts? How does the twain meet?
Richard: Great question. In the time I’ve spent in other countries with different healthcare models, I find they all have their intrinsic flaws. What you brought up is very basic and one-way, but cuts through all the other commentary about healthcare. It really gets down to a symptom-based healthcare system where providers make money on activity. If it’s that versus making money on hold, the whole outcome will always be the tension you just described.
The optimist in me is really encouraged by all the new value-based primary care provider organization like — Oak Street, etc. The leadership in those organizations is fantastic and trying to create the right kind of healthcare system for members — a 360 view. That will enable us to move forward in taking care of patients. Being a pharmacist, I saw there were many times I went back to your “do nothing” comment which has a lot of value and I agree with.
But we are making a choice for instance, on which five meds we can buy this week since we can’t afford all five. One’s for water intake so that can’t be dropped, the next is for pressure, else that’ll spike, the third is for diabetes and if sugar isn’t controlled, that’ll put you in the hospital and affect your feet, your eyes. All the drugs are important and having to choose is awful. If we’re just focused on that front then, we’ll have less people with diabetes and high blood pressure, people will make better food choices and start moving more. The entire healthcare system should be incentivized to drive that, not just the periphery organizations. It’s easy for me to say since that’s how I get paid but that tension will always be true.
The other thing that encourages me is that health systems also get this. Premier health systems are pivoting from big buildings with high towers and blinking lights and moving into more community settings and value-based arrangements or total cap risk. These types of things as CMS continues to incentivize that will make it possible for us to get there over time. But, will it be a 15 or 20 year vision versus a 5? I don’t know but it’s a real tension point.
Q. You’ve had a distinguished career in Walgreens and now you’re in a related business but what prepared you for your current role?
Richard: It’s my first time being a CEO, so till recently, I’ve felt that sometimes you just go by the seat of your pants. Walgreens is a really refined institution with smart people and world-class processes so my 28 years there gave me some unique capabilities to excel in my current role.
When I was working in stores as stock boy, cashier, photo clerk, pharmacy technician, assistant manager, pharmacist and then a store manager, I got the chance to help people, deliver a service to them and see the pain they underwent. What hit me hard was an episode in Minnesota where I was a district manager. I’d been waiting to shut the store, but the Front Cashier still had a few people in line. One of the ladies wasn’t buying anything but had been there for a couple of minutes and was explaining to the Cashier about her cat. I listened in and when I checked with the Cashier, I realised that the lady was here every day. She was lonely so the impact of that front cashier on this lady’s life was profound. Because of that I understood the humanity of living next to other humans who have different things.
On one of the panels, I was on, I heard someone say “we’re all in this together” — in this pandemic — but we all have different boats, yachts, families, wealth, a good home and there are those who are just trying to survive. I learned that being in retail, on the ground with patients pays me huge dividends today, because every time I make an executive decision, I put myself in that member’s shoes and check if this decision makes it better for that person. If the answer’s no, then, we’re not spending money on that. It’s hard to stay principled that way because you have shareholders and other competing priorities. But if you do that, it works out well for everybody.
Q. I can relate to that anecdote. I’ve realized through the pandemic; how every little thing makes a profound impact on somebody’s life when you don’t even know about it. There’s a great deal of resignation but also great opportunity, especially in healthcare. What is your advice to the younger generation that is coming into the workplace today and is looking at healthcare as a career?
Richard: I have three very simple things to say. One, pick a job where it makes a difference. Work in something that you have a passion for. Healthcare is mission-driven, our colleagues are so proud to work here and I’m impressed every day by the passion and commitment they have in the roles they play and in the difference they make. If you are passionate about helping people, addressing inequity, and improving the health of those around you, this is a great profession for you.
Second, the opportunities are limitless. We have a shortage of clinical people to deliver care in the future for this population. That means, there’s money and jobs available. I moderated a discussion about healthcare, workforce, and the need for clinical workers at all levels, recently, especially as we get out into rural America. But there are also these very innovative opportunities in digital health, data, health related services, mental health, senior living, home-based care etc. There’s a lot of M&A, money, finance, and banking. So, it makes a difference.
Third, learn about the aging space. This is a high need-high spend space. And all of us had a mom and dad and grandparents at some point. So, there’s so much innovation, need and jobs in the aging space. Nothing feels better than serving this population.
I got lucky because I discovered pharmacy. I got a job at a drugstore because I needed a pull-out CD player that my dad wouldn’t buy for me. When I fell upon pharmacy, it felt like I was giving back. Many young kids don’t always have the right opportunities because all that depends on your ecosystem — where you live and what you know of the world, which isn’t much when you’re young, even though a lot of time I thought, I knew everything. I learned over time that there’s so much you don’t know. So, I think it’s about the mission and the opportunity. The age-related space is cool for youngsters to get into.
We hope you enjoyed this podcast. Subscribe to our podcast series at www.thebigunlock.com and write to us at info@thebigunlock.com
Disclaimer: This Q&A has been derived from the podcast transcript and has been edited for readability and clarity
Recent Episodes
About the host
Paddy is the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy is also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He is the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He is widely published and has a by-lined column in CIO Magazine and other respected industry publications.