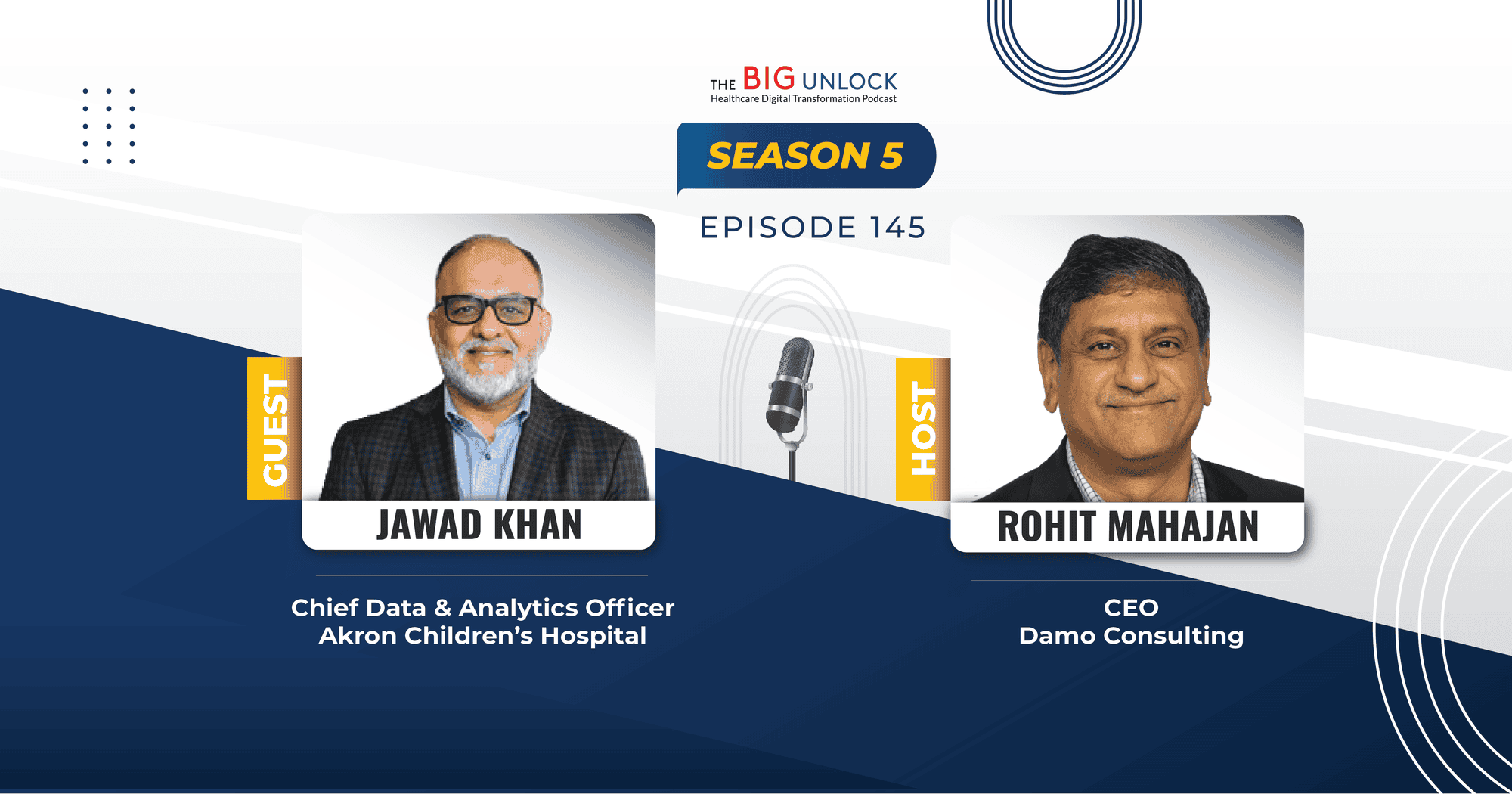
Season 5: Episode #145
Podcast with Jawad Khan, Chief Data & Analytics Officer, Akron Children's Hospital
Unlocking Healthcare Data from Proprietary Databases for Analytics is a Major Challenge
Share
In this episode, Jawad Khan, is the Chief Data & Analytics Officer of the Akron Children’s Hospital discusses his journey in healthcare and data analytics, focusing on digital transformation and the importance of data accessibility. He discusses several AI use cases in healthcare and highlights the critical role of data governance.
Jawad emphasizes on the importance of unlocking siloed data and utilizing it effectively to enhance care delivery for end users—both for patients as well as healthcare providers. He also highlights the use of GenAI to automate physician note summarization, reducing administrative burdens like “pajama time” while enhancing care. He stresses that while GenAI has several use cases, ensuring proper data validation and governance is critical to securely curate data before implementation.
According to Jawad, every challenge is an opportunity in healthcare. He also shares insights on fostering innovation and the potential future of AI in healthcare. Take a Listen!
Show Notes |
||||
| 01:14 | What interests you in the healthcare industry segment to become the CIO of a hospital system? | |||
| 02:47 | How long have you been in the leadership position at UMC, where is it located, and what kind of population does it serve? | |||
| 03:35 | You have done a lot of work from technology perspective to support the business needs of the hospital. You've done over 200 applications and transformed the EMR system. Would you like to share with the audience the thought process that drove those changes and what were some of those changes? | |||
| 07:47 | What do you think about your digital transformation efforts? If you could describe a few of them which have had impact on the patient population. | |||
| 08:30 | Please describe in your own, you know, way that what is digital transformation for provider systems such as yours? Where do you see it going? Some of the challenges that you might have faced and how did it actually end up impacting patients? | |||
| 11:24 | How did you manage to change the mindset of the people? How did they manage to change themselves? To adapt to this new world where technology, especially with AI and GenAI and other new technologies which are coming our way, how do you change mindsets and change behaviors and change culture over there? | |||
| 13:00 | Would you like to provide one example of how the technologies which you were implementing, and you continue to be implementing in your hospital system are accessible and usable by a variety of users, including within the hospital and outside the hospital. | |||
| 16:28 | How do you innovate? Do you involve external parties? Do you have some kind of a, you know, innovation focus department? Or is it part and parcel of everybody's, you know, kind of like daily life? | |||
| 19:24 | What are your thoughts on new technologies, especially Gen AI? Have you been experimenting with any predictive analytics or large language models? What would be your advice or thoughts to any other healthcare leaders on how to go about this journey of exploration? | |||
| 22:15 | Standing here now and looking back, if you were able to go back and change one or two things, what would you like to do differently or have done differently? | |||
Video Podcast and Extracts
About our guest
Jawad Khan is the Chief Data & Analytics Officer of the Akron Children’s Information Services Division. Previously, he was the chief analytics and data officer at Tufts Medicine in Boston, where his team supported the advanced analytics, business intelligence, quality, research and data governance vertices. Prior to his role at Tufts Medicine, Khan was the chief data architect for the Chicago Department of Public Health. He also served as the assistant vice president of advanced analytics and knowledge management at Rush University Medical Center, where he developed and executed data and advanced analytics utilizing AI/ML solutions, and delivered actionable data insights to clinical, research and university teams. Khan earned his bachelor's degree in computer engineering from Southern Illinois University.
Recent Episodes
Q: It is the 145th episode of the Big Unlock podcast, which the previous founder of Damo Consulting started five years ago. It is very well received in industry circles, and it’s great to have you as a guest on this podcast. Would you like to start with a brief introduction of yourself?
Jawad: Thank you so much for having me. I’m the Chief Data Analytics Officer and Vice President at Akron Children’s Hospital. I worked at Tufts University Medical Center prior to my job here at Akron, and before that, I was at Rush University Medical Center in Chicago.
I have over 15 years of experience on the provider side, working in data and analytics at different institutions. It has been an amazing journey. I’ve seen the progress and transformation within data and data infrastructure for analytics. It’s been exciting, and I’m happy to share my thoughts with you today.
Q: Would you like to tell us a little more about how you started in the healthcare provider industry? What attracted you, and what keeps you motivated today? And can you also tell us about the organization you work for, Akron Children’s, as you mentioned?
Jawad: Sure. Let me first start with the organization, and then I’ll talk about my background and how I got into healthcare and specifically data analytics in healthcare. Akron Children’s Hospital is the largest children’s hospital in Northern Ohio. We focus exclusively on paediatrics—children are our specialty.
We are a two-hospital system with three ERs, four urgent cares, and about 44 to 50 specialty clinics across Northern Ohio. We are a fully integrated system and use a single EHR across our health system, which is unique and serves us well as we continue to grow in the region.
A bit about me: I’m a computer scientist by background with a degree in computer engineering, and I also studied electrical engineering in college. My first job out of college was in healthcare IT. Back in the day, we were developing serverless Java applications for handheld devices, or PDAs, as they were called. We created applications for checking formularies for providers as they prescribed medications, faxing prescriptions to pharmacies, and other functions. This was in the early 2000s, so it was ahead of its time, but a great learning experience.
Since then, I started in healthcare IT but moved to various industries, working in marketing, real estate, and capital markets. I was the managing director of a capital markets company in the Chicago area. I then moved into enterprise architecture, doing a lot of cloud transformation work for a large company. Eventually, I had the opportunity to join Rush University Medical Center in the data analytics space as a director, later becoming EVP. Now, here I am, 15 years into healthcare systems, with experience through pandemics and other challenges.
Q: So, Jawad, when you think about digital transformation and how it’s solving challenges for your patient population, which is essentially, like you said, paediatrics and children in the local area, and perhaps people coming from all over the world as well, what are some of your thoughts? How do you approach it with your team at Akron Children’s? Any other experiences from your past that you’d like to share with the audience?
Jawad: Our mission at Akron Children’s is to do everything for them that we would do for our own children. So, we don’t turn anybody away. That’s part of our core values and mission of the organization, and we’re very sincere and focused on that, on delivering value and fulfilling our mission. What that really means is our objective is always to provide the best possible care.
We always look at holistic care. We have several programs anchored in the community and in schools where we focus not just on sick care but also on wellness care. We want to make sure our patients stay healthy and remain healthy for the rest of their lives. And these are kids we’re dealing with, so we are very, very passionate about that.
Q: When you think about some of the challenges in the digital transformation space from your perspective as a children’s hospital, what are your thoughts? What are the initiatives or projects you’re currently working on, and what do you have in mind for the future?
Jawad: One of the challenges, and all challenges are opportunities eventually in healthcare, is that data is often locked in proprietary databases. At Akron Children’s, we’re fortunate because we’re an integrated system with a single EHR across our entire system. It’s a bit easier from the EHR perspective, but EHR is just one application among 300-odd applications that make up our entire IT ecosystem.
All of those systems collect data, and that data is critically important. It’s very difficult for any institution, including ours, to unlock all of that data, convert it into information, and eventually generate knowledge that can be leveraged. So that’s a very current and ongoing challenge. We’re looking at several ways to ensure we can extract data from all relevant applications needed for data analytics. We want to provide that data to the right people, who can then extract knowledge and make data-informed business decisions.
For the last 15 years, there’s been so much change in that space. We used to manage data in siloed databases. But now, we’re talking about integrating it into open platforms, like public cloud, using Lakehouse architectures to bring data together. The goal is to make data easier to access and remove as much friction as possible in making that data available to end users. It’s been a journey, and it continues to be a journey.
Q: When you say end users, are you also thinking end users in terms of the patients themselves for self-service applications? Or mostly when you’re thinking end users, you’re thinking of the application systems within the hospital that your colleagues, physicians, and nurses might be using?
Jawad: We are thinking all of the above. Today, patients can access their data within minutes of their visit. Labs become available to them on apps as soon as they get their labs done. So yes, we are providing access for our end users—patients—to the data in a timely fashion.
We are also talking about internal customers who are responsible for running the business. We are accountable for ensuring the system runs on data-informed decisions. So, all of that is part of our end users, and we strive to provide data to them by removing all obstacles and friction, organizing the data in a meaningful, usable way.
Q: How do you wrestle with the challenge of when someone comes in from another hospital system that may not have the same EMR or EHR? Do they still bring their health record along with them, or do you have to request it from the other health system? How does the whole process work in terms of data platform interoperability?
Jawad: It has improved quite a bit. If folks come from hospital systems using one of the current EHRs, since we are an Epic customer, we have care everywhere in our backend to exchange data between Epic hospitals and even some non-Epic hospitals that participate in that network. We have backend capabilities that allow us to exchange information between systems.
Now, not everyone is part of that network or can share information programmatically in a timely fashion. When that falls short, we use older methods—calling on behalf of the patient, receiving data in CDC format, or even just a fax that gets scanned into our EHR, making the data available.
Yes, over time, it has improved, but we still rely on legacy methods that aren’t timely. There can also be compliance issues depending on the state, and patient consent is required, which can create obstacles. But we are able to exchange information using both advanced and older methods.
Q: Before I move on to more exciting technologies like AI and GenAI and how you’re thinking about those use cases, I want to touch upon innovation. How do you foster innovation in a large health system where clinical decisions impact patient care? Any thoughts or examples from either your current or previous experiences?
Jawad: Yeah, that also is an art and exercise in itself. There’s a lot of innovation happening now, and healthcare is at an influx point. Historically, healthcare has lagged in adopting innovation compared to other industries, but with GenAI and AI, it’s starting to leap ahead. I’m excited that healthcare is ready to accept innovation and address the challenges it can solve.
At Akron Children’s, we’re using GenAI for note summarization for physicians to reduce pajama time, meaning time spent outside clinical hours completing summaries of visits. GenAI was able to summarize them and even do other additional things to make it more time efficient for them to be able to document. Documentation is a big burden on healthcare and healthcare providers. Gen AI is obviously a very natural use case.
There are other areas, where automation and AI is becoming quite relevant and important, including pre-authorizations, where I’m seeing a lot of implementations on inbox management. Inbox management has been always been a burden for the providers. Automation of routing of messages, even auto replying some of those messages, obviously with human in loop to make sure that they are able to physically read the message that was generated, authorizes, and send it forward. These are the very low hanging fruit in terms of how GenAI is implemented. We are using data and analytics side also.
There is quite a bit of GenAI applications that I am seeing now. We haven’t implemented them yet, but we’re in the process of evaluating them and implementing them for folks to be able to use natural language process, like natural language to extract insights from the data.
You can come to the data and you can ask the question in your most comfortable language using your most comfortable phrases and the GenAI then provide the dashboard without anybody having to create a dashboard. Analytics is also becoming quite common now.
We are actually piloting it to implement it at our institution as well. GenAI is also being used in the background which front end users might not be able to see. To normalize the data, to curate the data, there’s a lot of solutions that we’re piloting and evaluating. We are working with various partners to see how it would make our processes or back-end processes effective.
This is a high interest of us right now because that directly translates to FTEs, that really translates to ROI, and things that we do, and even improved efficiency, integrity, and quality of the data as we look forward. So, I’m very, very excited about these solutions.
Q: That’s great to know. New technologies like GenAI often come with governance challenges. Could you share how you approach data governance in your organization, especially in the context of AI?
Jawad: Yeah, we should all remember that Gen AI is not an exception. Of course, we can discuss the risks of Gen AI and AI in general, but ensuring proper validation, data quality, and care quality has always been central to healthcare. We are a regulated industry, and we must make sure that since we are dealing with human lives, all healthcare solutions are validated, curated, secure, and have been thoroughly tested before they are implemented. This applies to any healthcare innovation.
With Gen AI, given that it’s artificial intelligence and involves machine learning, there are some added risks that require validation, like understanding the openness of the model and how interpretive it is. These aspects are critical. Regarding governance, when it comes to implementing AI or even non-AI innovations, we have established proper committees. We have an AI committee that reviews all proposed solutions. The team of informaticists carefully evaluates and validates these solutions to ensure they are feasible for implementation.
We also have a data governance structure in our organization with a steering committee and a data analytics committee. They oversee data curation processes, data definitions, and the validation of metrics. What I’m getting at is that we manage the entire end-to-end lifecycle of data—data and analytics. When I say analytics, I’m also referring to advanced analytics, including predictive modeling and machine learning, which all fall under the purview of our AI committee.
Members from various parts of the organization sit on this committee. Our Chief Informatics Officer leads the initiative from the Information Services Department. I am also a member, along with our CISO and key clinical staff, to ensure that new technologies are fully understood and vetted before they are implemented.
We have governance structures in place, and whether we use them effectively is something time will reveal. As new solutions and innovations are introduced, we will refine and adapt these processes as needed. But we do have a solid organization in place to implement AI innovations, and that’s reassuring.
Q: Any parting thoughts or suggestions for the audience on what you’re seeing for the future?
Jawad: If I summarize my 15 years in data analytics, especially in healthcare, the challenge is dealing with data and unlocking silos. Today, 80-90% of our analytics is generated using only 20% of the data. A lot of data is unused so as we look forward to sort of turn the curve on this, we really have to understand the best possible ways to be multi-modal in our approach to solutions.
So how do you not just do with discrete data? What do you do with unstructured data? What do you do with imaging data? All of these solutions, like we have to think through those things more carefully and not leave them behind, right? Not leave the 80 percent data behind to provide majority of the solutions.
We have to start becoming more data-savvy and multi-modal in our approach, considering not just discrete data but also unstructured data and imaging data. That’s really what we have been dealing with as we build warehouses, they cause us. The idea really becomes, how do you model the data?
My other recommendation to your listeners would be to adopt common data standards as much as possible. Whether you are good in FHIR schema or whether you want to go more on the research side and implement OMOP like, uh, schema to organize your data, all of those solutions are feasible and staying to the common data standards might help down the road as you exchange and become more interoperable with other institutions.
Also, think about how to present your data through APIs so that apps can consume it easily. Removing friction in data access will be key moving forward.
Today, most of the good innovations are happening on the app side, so apps are being developed that are more transactional with the data. So, how do you present the data as application programming interfaces or APIs so that those apps can consume your data? These are the things that we really have to think about and organize the data so that it becomes like we remove all the frictions for folks to access the data.
We hope you enjoyed this podcast. Subscribe to our podcast series at www.thebigunlock.com and write to us at info@damoconsulting.net
Disclaimer: This Q&A has been derived from the podcast transcript and has been edited for readability and clarity.
About the host
Paddy is the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy is also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He is the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He is widely published and has a by-lined column in CIO Magazine and other respected industry publications.
About the Host

Ritu M. Uberoy has over twenty-five years of experience in the software and information technology industry in the United States and in India. She established Saviance Technologies in India and has been involved in the delivery of several successful software projects and products to clients in various industry segments.
Ritu completed AI for Health Care: Concepts and Applications from the Harvard T.H. Chan School of Public Health and Applied Generative AI for Digital Transformation from MIT Professional Education. She has successfully taught Gen AI concepts in a classroom setting in Houston and in workshop settings to C-Suite leaders in Boston and Cleveland. She attended HIMSS in March 2024 at Orlando and the Imagination in Action AI Summit at MIT in April 2024. She is also responsible for the GenAI Center of Excellence at BigRio and DigiMTM Digital Maturity Model and Assessment at Damo.
Ritu earned her Bachelor’s degree in Computer Science from Delhi Institute of Technology (now NSIT) and a Master’s degree in Computer Science from Santa Clara University in California. She has participated in the Fellow’s program at The Wharton School, University of Pennsylvania.
About the Host
Rohit Mahajan is an entrepreneur and a leader in the information technology and software industry. His focus lies in the field of artificial intelligence and digital transformation. He has also written a book on Quantum Care, A Deep Dive into AI for Health Delivery and Research that has been published and has been trending #1 in several categories on Amazon.
Rohit is skilled in business and IT strategy, M&A, Sales & Marketing and Global Delivery. He holds a bachelor’s degree in Electronics and Communications Engineering, is a Wharton School Fellow and a graduate from the Harvard Business School.
Rohit is the CEO of Damo, Managing Partner and CEO of BigRio, the President at Citadel Discovery, Advisor at CarTwin, Managing Partner at C2R Tech, and Founder at BetterLungs. He has previously also worked with IBM and Wipro. He completed his executive education programs in AI in Business and Healthcare from MIT Sloan, MIT CSAIL and Harvard School of Public Health. He has completed the Global Healthcare Leaders Program from Harvard Medical School.
About the Legend
Paddy was the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy was also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He was the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He was widely published and had a by-lined column in CIO Magazine and other respected industry publications.





 Hosted by Rohit Mahajan
Hosted by Rohit Mahajan