AI is having a transformative impact on the pharmaceutical industry. The use of AI tools is dramatically accelerating clinical trials the drug discovery process by drastically cutting time and costs through predictive modeling, virtual screening, automated labs, identifying novel targets, predicting compound properties and even repurposing existing drugs, making the process faster, more efficient, and personalized by analyzing vast biological datasets to find better candidates and pathways.
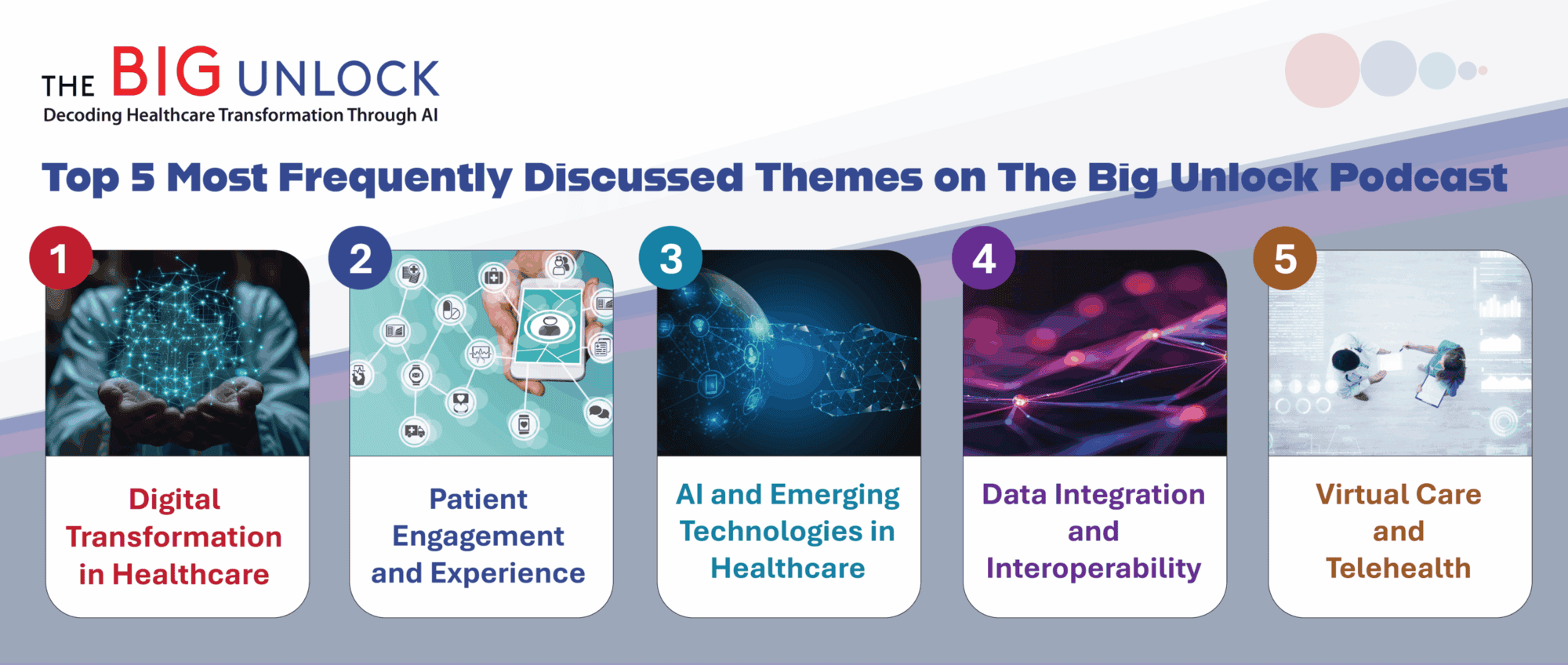
On a recent episode of The Big Unlock podcast Gregory Goldmacher, M.D., Associate Vice President in Clinical Research, and Head of Clinical Imaging & Pathology at Merck Research Laboratories sat down with host Rohit Mahajan, Managing Partner at BigRio and Damo to discuss how AI is improving drug discovery and the challenges that still remain.
Dr. Goldmacher first discussed how we all know that clinical trials are very expensive and time-consuming and how there are many ways that AI can reduce both of those burdens. “AI essentially improves efficiency, which means it can accelerate every aspect of a clinical trial. In the preclinical phase, AI is being used for things like genome searches and for target identification. When it comes to drug design it can help assess molecular protein interactions and things of that nature, and in the clinical space there’s a lot of use of AI to support clinical operations. That includes things like creating documents, protocols, clinical study reports, informed consent forms, reports of various kinds.”
He went on to discuss that in every clinical trial there is a massive amount of data that gets collected and manual review of all that data is extremely labor intensive. He explained to Rohit that both “traditional AI” and newly introduced “AI agents” can absolutely help sort through this enormous amount of data for targeted analysis.
AI, Drug Discovery and Endpoints
Dr. Goldmacher described endpoints as the core of every clinical trial, since they determine whether a therapy is safe or effective. As he told Rohit, “Endpoints are measurements. Drug trials require accurate measurements to make decisions. AI allows us to make better measurements for better decisions. He went on to illustrate with an example from his own background in medical imaging.
“Let’s take cancer as an example. The traditional way of assessing whether a cancer drug is working in a clinical trial is that you do a scan, let’s say a CT scan before treatment starts. You identify the tumors, and you pick out a few of them that you’re going to measure. Imaging continues over the course of the trial, and if the measurements shrink, that’s called a response. That’s good if they increase, that’s called progression, which is bad. What you do at each assessment point is apply a mathematical algorithm to each tumor you are tracking to determine if you are getting a complete response, a partial response or no response or progression. Then you look at all those responses, and you extract an endpoint such as objective response rate or progression-free survival based on established criteria.”
He then discussed where AI comes in, particularly when it comes to medical imaging. He explained to Rohit that in those initial scans, there is a lot of information that isn’t immediately visible to the naked eye. AI models can see patterns, pixel patterns that indicate a lot more than just how big a tumor is, but its microbiology, such as invasive vascularity or necrosis, any number of things that are not appreciable with the eye, but can be measured by a model and tracked via AI that can look for those patterns and assess a drugs specific effectiveness on a specific immuno-oncology response and not merely if a tumor has grown or not.
“In that initial scan traditionally, you are only measuring size and using that as your endpoint. There is so much more info there that could make for a more efficient trial, however human analysis of those scans to determine the tumor microenvironment is extremely expensive and time consuming -for radiologists — but not for AI.”
What the Future Holds for AI and Drug Discovery
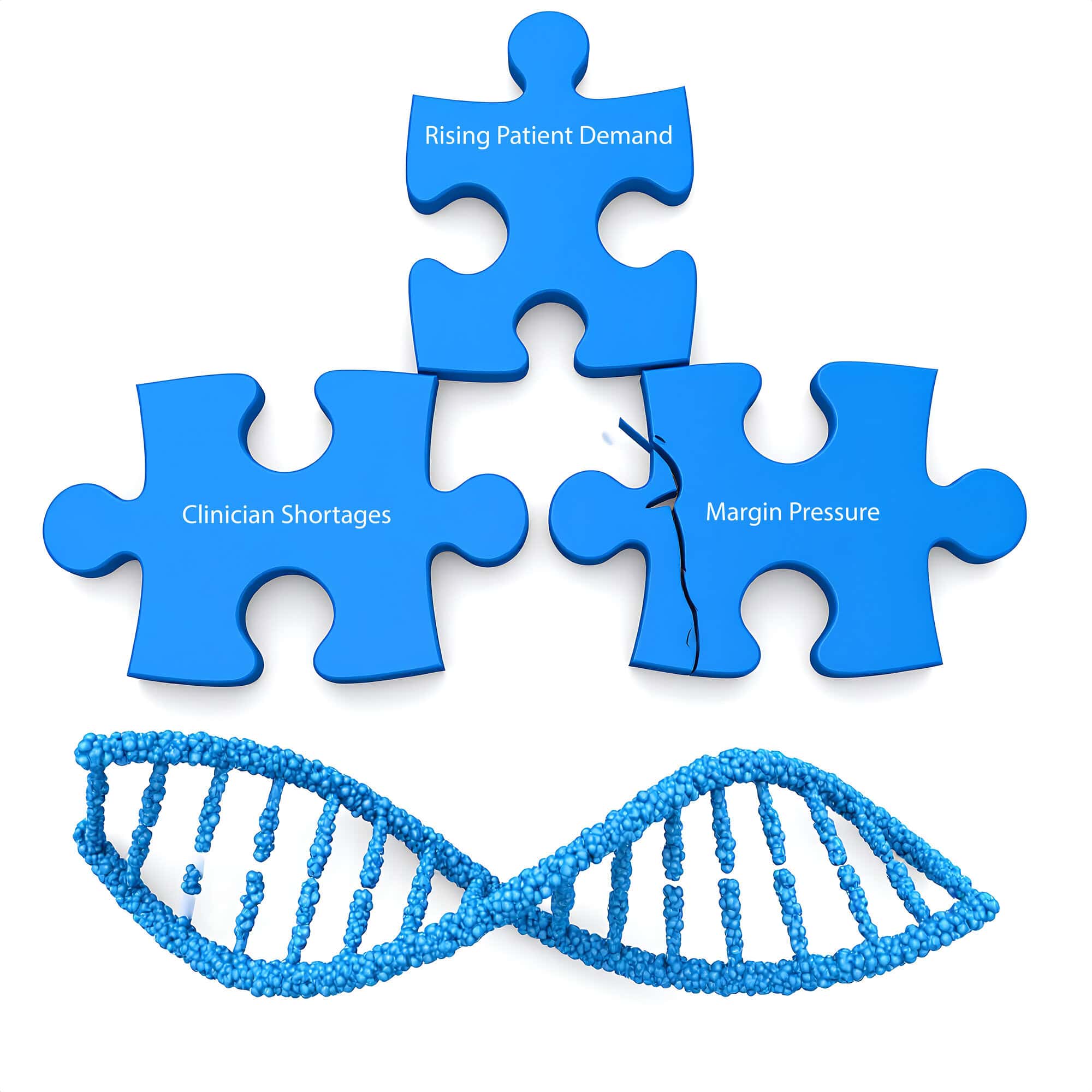
Despite the obvious increases in efficiency that AI tools can bring to clinical trials, Dr. Goldmacher cautioned that challenges remain, mostly surrounding Big Data and privacy issues.
He stressed that drug development still depends on huge volumes of data spread across legacy systems. Without strong data standardization, even the most sophisticated AI tools cannot deliver reliable results. As he concluded his interview with Rohit, Greg pointed to the FDA’s evolving guidance on AI and emphasized the need for rigorous validation before using AI-derived measurements for all regulatory decisions, but underscored that with thoughtful adoption, AI can support better decisions in clinical development and improve outcomes for patients. Take a listen to the entire podcast here.