Season 7
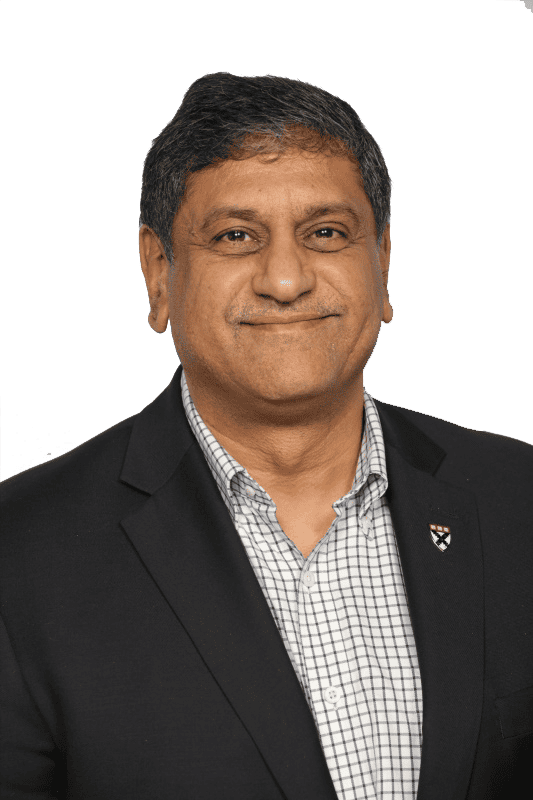
Episode 194 - Podcast with Chethan Sathya, MD., Vice President of Strategic Initiatives, Northwell Health - AI Succeeds Through Seamless Workflow Integration and Clinician Empowerment
In this episode, Dr. Chethan Sathya, Vice President of Strategic Initiatives at Northwell Health, unpacks why healthcare innovation only scales when clinicians, public health, and AI are designed to work together.
Dr. Sathya shares his journey from surgery to journalism to public health advocacy, including leading gun violence prevention efforts. He explains why most AI pilots fail, because of poor workflow integration and clinician burden, and why ambient intelligence, tele-specialty care, and agentic AI are poised to scale. His message is clear: build technology alongside clinicians, not around them. Take a listen.
About Our Guest

Chethan Sathya, MD, MSc is a pediatric surgeon, public health leader, journalist, and Vice President of Strategic Initiatives Northwell Health. He has received numerous awards and recognitions, including top 40 under 40 by Modern Healthcare, the Community Health Leadership award from the United Hospital Fund, and Top Rising Healthcare Leaders Under 40 by Becker’s Hospital Review. As Director of Northwell’s Center for Gun Violence Prevention, he spearheads an innovative, health system-wide approach to firearm injury prevention, integrating research, clinical screening, advocacy, and public health interventions. Dr. Sathya has received grants totaling more than $5 million and has published numerous peer reviewed papers that have helped significantly advance the fields of injury prevention, pediatrics, implementation science, and public health.
A National Institutes of Health (NIH)-funded researcher and reviewer, Dr. Sathya led the development of a pioneering universal screening protocol for firearm injury risk, through which over 100,000 families have been screened. He also founded the National Gun Violence Prevention Learning Collaborative, engaging over 600 healthcare institutions in evidence-based firearm injury prevention strategies. His leadership extends to national partnerships, including the Milken Institute (Senior Advisor), the Clinton Foundation, Sandy Hook Promise (Board of Directors), and White House-led health system convenings on gun violence prevention.
Beyond firearm injury prevention, Dr. Sathya has been at the forefront of public health and healthcare innovation. He has led system wide initiatives in health disparities, childhood disease prevention, social innovation, and value-based care, and has also worked closely with state and federal agencies and lawmakers to improve public health infrastructure, re-think private-public partnerships, and leverage unique aspects of social innovation to improve health outcomes. He also advises startups and major health tech firms on AI in medicine, digital health, and data-driven solutions. With expertise in implementation science, he focuses on scaling and sustaining innovative healthcare strategies.
A sought-after thought leader and surgeon-journalist, Dr. Sathya has contributed to CNN, Scientific American, The Washington Post,and TIME and has delivered keynotes at major forums including the World Economic Forum, Clinton Global Initiative, Milken Global, the White House, American Hospital Association and the National Academies of Sciences, Engineering, and Medicine. He also serves as Trauma Director at Cohen Children’s Medical Center, Associate Professor of Surgery and Pediatrics at the Zucker School of Medicine, and Affiliate Scientist at the University of Toronto. Dr. Sathya completed his undergraduate degree at McGill University, medical school and general surgery training at the University of Toronto, followed by a Pediatric Surgery Fellowship at Northwestern Medicine in Chicago. He holds a Master’s in Clinical Epidemiology from the University of Toronto and completed a Fellowship in Global Journalism at the Munk School of Global Affairs. Additionally, he pursued a Public Health program at the Dalla Lana School of Public Health and completed the Health Policy and Executive Leadership program at the Heller School for Social Policy and Management at Brandeis University.
Recent Episodes
Charles: I am Chuck Christian. I’m the Vice President of Technology and CTO for Franciscan Health. Franciscan is a 12 or 13 hospital system, depending on how you count them. We cover a swath of the Midwest from just south of Indianapolis all the way to Chicago, basically following the I-65 corridor.
We have between 350 and 400 locations, including physician practices, imaging centers, lab draws, urgent cares, and oncology centers. It’s a pretty large organization. We have about 29,000 team members, both employees and contractors, at Franciscan Health.
We are truly mission focused. We are a Catholic healthcare system with a big C. We are owned by the Sisters of St. Francis of Perpetual Adoration. That means there are two sisters in the chapel praying for whatever they deem important and anything we ask them to pray for, 24 hours a day, seven days a week, 365 days a year. That’s where the “perpetual adoration” comes in.
We are a mission-driven organization. I believe in that. A lot of our hospitals are smaller and in underserved places, and we take care of that patient population. I think we’re really good at it.
I’ve known this organization almost 40 years. The CIO previous to Charles, who is our current COO, was a good friend of mine. I was CIO of a hospital in Southern Indiana for 24 years, and Bill and I ran a similar software stack. I watched Bill and learned a lot from him as far as how he ran this large organization.
I’ve been here for six years. I joined in April of 2019, so in dog years that’s like 35 years or more. We are very busy. I’m very blessed to have an outstanding team that manages all this, and I get to stand in awe and watch everything we accomplish every day.
Rohit: That’s fabulous. Thank you, Chuck for that intro.
Ritu: My name is Ritu Roy, and I’m the Managing Partner here at Damo and BigRio, and also the co-host of The Big Unlock podcast with Rohit. Thank you for being our guest today, Chuck. We are looking forward to an engaging and insightful conversation. With that, we can dive right in and get started.
Charles: Thank you.
Rohit: Hi Chuck. I’m Rohit Mahajan. I’m the Managing Partner and CEO at BigRio and Damo Consulting. It’s great to have you on the podcast. Like Ritu said, we’re looking forward to an engaging discussion. I’d like to start with the first thought on my mind. You’re in a mission-driven organization, and you’ve been a healthcare leader for many years. What started you on this journey? Tell us how you got started in healthcare, what attracted you, and what you’re passionate about.
Charles: Well, it depends on how far back you want to go. I’m an X-ray tech, radiologic technologist if you want to use the term. The first 14 years of my career were in radiology.
I stepped out of high school on June sixth in 1971, and on June seventh I stepped into the hospital, and I haven’t left since. Interesting enough, I did a lot of things in the radiology department and became part of the management team of that department. I guess if the chief tech had not been just a few years older than me, I’d still be there, because that was the role I wanted. But Roy just retired a few years ago, and I wasn’t going to wait that long.
I’m a geek, I’m a nerd. I was a nerd in high school. It wasn’t cool to be a nerd in high school back then, but it’s cool to be a nerd now. I did a lot of programming classes on the old System Threes with punch cards. Then I learned how to code for Z80 processors.
When we started automating hospitals back in the mid-eighties, I got chosen to run the ambulatory implementation of order management after we had put in patient management. I realized I liked it, and I knew that was where healthcare was going. Radiology has been a high-tech department in hospitals for a long time. I was trying to automate the patient record in radiology, but it was so expensive I couldn’t get any funding for it.
So I jumped ship and moved over to the vendors for about five years. Eventually I was asked to move to either an implementation manager role or the director of an outsourced IT department in southern Indiana. I did that. I had four daughters at the time, and it was the right thing to do because it was a great place to raise my girls.
I spent 24 years there. It was during the time the role of a healthcare CIO was defined. When I left that job, I was Vice President and CIO. I moved to Georgia to a health system there as Vice President and Chief Information Officer. Then I came back to Indiana and worked at the Indiana Health Information Exchange, which is now the only exchange in Indiana. I had been involved with it since 2005. I worked there for a little over four years, and then I took this role here. That’s my stint in healthcare, which has spanned over 50 years.
Rohit: That’s awesome, Chuck. You’ve been there, done it, and seen it as well. I was curious because a few days ago, when we were chatting, you were talking about being either back from UGM or about to go there.
We all know it’s a week-long affair, people go deep, and there are so many things to cover. We were wondering if you could share some of your experiences or a heads-up on topics you see coming our way.
Charles: Sure. I came home with a great deal of anxiety because of trying to figure out how we’re going to do everything and where healthcare is going. The nice thing about Epic is they now cover the entire gambit. I remember when Epic started; they were only in the ambulatory space and then only in large academic medical centers. They cover quite a scope of product these days.
Now that they have grown the applications, they have de-identified shared data, which I think is going to be a plus. The two-letter acronym was everywhere, AI, and how it’s going to be leveraged and used. They did a nice job showing scenarios of how it could be used and how organizations are using it.
We’re a risk-averse organization. We’re taking a more moderated approach. We’re getting our governance in place first. We already have a few things going through the AI mill, and we will have more. We split it into two pieces, one on the clinical side and one on the operational side. Epic has both, and I think they’re well positioned to do that work. They partner with Microsoft, and they continue to do so.
They announced they are working on their own ambient listening. They have business partners already, but they are creating their own product. I assume it will be predicated on the Microsoft stack, but they didn’t say, so I don’t know.
They also mentioned they are working on their own ERP and starting with workforce management. That makes sense because the workforce is in Epic all the time. Nursing staffing, scheduling, shifts, and how all that ties together. It’s an interesting leap.
Years ago, when Lawson, before being purchased by Infor, said they would create a patient accounting platform, I was in a CHIME focus group. When they mentioned that, a bunch of CIOs in the room asked why they would do that. You need to get your ERP right first. But I think the way Epic is approaching it makes sense.
It was great. I was there for about four days and spent most of the time listening to presentations. Judy did a great job with a big screen about what’s next and what’s coming. The rest of her team did a great job showing what you can do now and what’s coming. They do a good job setting expectations around timelines. They release quarterly. We do two a year, so we’re current from their perspective but behind. We don’t have the wherewithal to immediately adopt everything when they release it, so we have to plan accordingly.
Ritu: Yeah. So Chuck, when I was reading about the UGM, it was interesting because they said their unique proposition with AI is the de-identified patient records they have in Epic Cosmos, which is more than 15 billion patient records. They said that for the first time, it can actually move toward healthcare rather than sick care because doctors can predict trends. And I think they released two new things called Emmy and Penny, which will help doctors see the trajectory of what is going to happen with patients.
So I was curious about your thoughts because you’ve been in this industry for such a long time. Do you think that this USP—this huge bank of patient records—is really going to set them on a differentiating path compared to all the other AI startups trying to do the same thing?
Charles: I think that having the data is huge, honestly. It reminded me a lot of—if you remember years ago—they had a thing called PatientsLikeMe, where people with unique and rare diseases could find others and compare notes and treatment approaches. Working at the Indiana Health Information Exchange, I know they have about 30 years of data. Not all of it is discrete, but the majority is.
One question I asked the CEO, who is a friend of mine—and a lot of researchers use that de-identified data—is that when you create an AI model and just let it learn, there are all kinds of interesting determinations you can make once you have the data. So I think it’s going to be a game changer. Epic is also trying to outdo themselves. Given the market of EHR vendors, there aren’t many left standing. There are three or four. Others are creating similar repositories, but I’m not sure they have the long-term vision or the wherewithal to get it done. Knowing the talent Judy has pulled together, I think it will be very interesting to see what comes down the pike.
Ritu: Thank you.
Rohit: Chuck, you mentioned you’re taking a conservative approach to AI adoption and setting governance before taking major steps. How do you think about innovation or typical problem-solving—for example, reducing cognitive load across the organization? How do you balance this conservative approach with the fast-paced changes happening in the marketplace?
Charles: I think we have to be very clear about what problem we’re trying to solve. There are so many solutions being thrown at us—“Hey, we can do this, we can do that”—but often it’s not a problem we actually have. So we’re trying to pick and choose which targets to shoot at.
I’m married to a critical care nurse, so I’m very careful about getting in the way of the nursing staff. She’s retired, but for me, technology needs to be invisible. If it gets in the way of people being able to do their job, then it’s a problem.
If you think about it for a minute—and I’ll give you Chuck’s opinion—we don’t really have electronic medical record systems for documenting the care of the patient. What we have are electronic systems that capture information required for billing. That’s part of the problem. We have all these required elements clinicians have to document—physicians have to dot all the i’s and cross all the t’s—to get the appropriate words in so it can be translated into billing codes, ICD-10 codes, HPS codes, and so on. It truly gets in the way of taking care of patients.
But once we get that discrete data, we can use AI and other tools to help determine a better course of treatment. You’re never going to hear me say that we should depend solely upon AI. It has to be moderated and reviewed by someone with clinical training. Physicians have shown me I’ve been wrong more times than you can imagine. Working together and having good data aggregation is important.
One thing I learned early on when implementing the first physician order entry and clinical documentation systems was that physicians said: “Don’t tell me what I already know. Tell me what I don’t know. Better yet, tell me what I need to know about the patient in front of me right now.” There are things they don’t know. That’s where data aggregation from health information exchanges helps, because patients don’t get care in one location or from one physician.
I’m living proof of that. I get care in two—actually three—health systems because that’s where my specialists are. My primary care doctor wants to know what my orthopedist did or what my cardiologist’s course of treatment is, because he’s managing my diabetes and a few other things. Having access to information—recent labs, imaging studies—is extremely important.
We talked about interoperability, and that’s where it comes into play. Most hospitals in Indianapolis are on Epic, so you can get data easily. From non-Epic systems, there are mechanisms too. When I see my cardiologist—who uses a different system—and he already knows what my medications are because they were recently changed by another physician, that’s positive. I don’t have to list everything. When they know my latest labs, that’s positive too, because we’re not hunting for information.
It’s about providing information that is important to the treatment at that moment.
I had the privilege of sitting in a presentation—maybe eight or nine years ago—at Scripps Institute. They showed a demo of what a patient encounter could be. It was very Star Trek–like. The computer or AI interacted with the physician and patient appropriately. It listened in the background and captured information about the encounter. When the physician said, “We need to order a CT scan of your lower abdomen,” it was already getting that scheduled. When the patient was ready to leave, everything was set. It was also checking for recent labs and reminding the physician if the patient—say a diabetic—was due for an eye exam or foot check.
I think it’s about having access to the information so we can inform—not determine but inform—the physicians. Because at the end of the day, physicians are accountable for the outcomes. They have to be in control, not the AI.
Ritu: Yeah,
Charles: we’re not ready for Skynet yet.
Ritu: I think you described a multi-agent system where the agents are off doing things and then bringing it all back for the physician to review. With that being said, we all know that AgTech is one of the top trends everyone’s talking about these days. What are your thoughts on voice agents? Where is Franciscan with that? Have you had exposure to or tried voice agents in the hospital?
Charles: Yeah, we’ve got a trial. We’ve got over 200 physicians working on those. Is it going to be the end-all, be-all? I don’t know. The physicians seem to like it. It assists them; it helps with their pajama time.
I’ve listened to conversations from other health systems that were early adopters, and I have to go back in time to when we were looking at automating physician practices in Southern Indiana. We visited a group of 14 family practice doctors. The husband and wife who started the practice mostly did OB and family medicine. Their use of computers was minimal—they were still mostly on paper. But they had other physicians who, I think, slept with their laptops.
The interesting thing was that depending on how well a physician adopted the computer system and molded it to how they practiced, they got to take advantage of it. I think it’s going to be the same with AI and voice agents. If they allow it to help and figure out how to incorporate it into how they think and practice, they’ll see the benefit. The systems are pliable enough now that it’s easier to do.
When I was in Georgia, we needed to automate a lot of OB practices on the same platform. One OB had been practicing almost 30 years and already had a solution he had customized. He told me I would tear it out of his cold, dead fingers. So we worked with him. The new system was more flexible and pliable than his old one, and he became a champion because he was willing to take the time to understand how he could use the technology to help him practice.
I think that’s the key. If you’re resistant to it, that’s fine—that’s perfectly okay. But people who write software often think all physicians think the same way. They’re absolutely wrong. It depends on where they trained. I learned that when implementing emergency room electronic medical records. The physicians who helped design the software were trained with a very different approach to critical thinking than our physicians. We had to relearn and figure out ways to adjust, because once clinicians are trained a certain way, it’s hard to change those habits and the way they gather and maintain information.
Ritu: Thank you. Great answer.
Rohit: Chuck, I’d like to ask your thoughts about the innovation process. How do you approach it, and what are some of the things you do to foster innovation?
Charles: One of the things we did was stand up a Tech Innovation Lab. Honestly, it was a selfish move because people were just bringing technology into the organization. All the enterprise architects report to me, and we work together to understand what will work in our environment and what won’t. We try to standardize as much as we can.
So I created the Innovation Lab to bring these innovations into a controlled environment and try them there. It’s a walled garden. It’s not connected to the rest of the network. It has its own connections to the internet. So if we blow something up, it only blows up in the lab. That’s why we did it.
What we’re able to do is bring ideas in and fail fast—figure out what works and what doesn’t. We’ve done that several times. Virtual nursing is something we’ve worked on a lot. There were all kinds of interesting opportunities brought to us. One facility went ahead and put a solution into a live patient population, and we found out quickly that’s not how you do it. You don’t test that kind of thing in a live environment. It frustrates the staff and patients, and it leaves leadership thinking, “We already tried that—it doesn’t work.”
Well, you tried what doesn’t work. Let me show you what will work.
We needed the opportunity to rapidly figure out what would work. One issue with that failed experiment was that the people who built the carts didn’t understand our environment. They put a wireless access point in the cart that was incompatible with our network. Once we got the cart, we figured it out quickly. We re-engineered it, and it works fine now—but we’re not using that cart because it was over-engineered and very expensive.
We’re trying to use standard components that can be supported and replaced quickly. The idea is to generate a lot of ideas and figure out how to use them appropriately without getting in the way.
You also have to think about the aesthetics of the equipment you’re bringing in. The first cart had a big five-wheel base—kind of a star shape. In some patient rooms, it was in the way. Nursing quickly said, “That’s not going to work.”
So we found an iPad holder that hangs on the patient’s bedroom wall when not in use. It’s out of the way, easy to access, and uses magnetic connectors so if someone snags it, it just comes apart. No trip hazard.
You must consider not only the technology but how it fits in patient rooms.
Originally, the idea was that the Innovation Lab would review the technology, understand how it fits together, and then install it in our SIM labs. We have two—one north, one south. Then the simulation teams would put it in a physician office or patient room and see how it fits before we use it in live care. That’s our next step with virtual nursing.
We also have a lot of conversations with organizations that have fully rolled out these solutions. We learn from their experiences. A mistake is only a mistake if you don’t learn from it. If you do, then it’s experience. We leverage their experience so we don’t repeat the same things, and so we can move quicker.
Rohit: That’s awesome. As we are approaching the end of the podcast, I would like to ask if you would touch on the mentorship program.
Ritu: Yes, I would really like to hear more about that, Chuck, because it’s something unique and I think it would be interesting for our listeners as well.
Charles: Just making sure we’re talking about the virtual mentoring program. After COVID, we were bringing on a lot of new nurse graduates. When you bring someone into that role, they need a more experienced nurse for a procedure they may have never done before. That usually means waiting for that nurse to come to them.
We had a couple of nursing staff in the mentorship program who came up with a way to use technology for an on-screen virtual visit with the new nurse. The experienced nurse could walk them through the procedure and be there with them, or if the new nurse had a question, they could step out into the hall, ask it, and go back in. It improved speed to delivery of care more than anything else.
It also gave seasoned nurses a chance to step away from what they were doing instead of traveling to another location. If they need to go in person, they still do, but this gave us another option. We got great feedback from both the new nurses and our more mature nursing staff, and we rolled it out through the enterprise. I haven’t checked in on it recently, but I assume it’s still running. I only hear when things break, and if it’s not broken, I’m not going to fix it. I assume the technology is still working and paying dividends.
Ritu: Thank you so much.
Rohit: So, Chuck, as we come to the end of the podcast, any closing remarks or thoughts you’d like to share before we finish?
Charles: I’ve been in healthcare a long time. Healthcare is a target rich environment for creativity and innovation. But we’re still taking care of patients the same way we did, and it’s about the human touch and caring for people.
When I first started in radiology years ago, I was taken aback that people weren’t always treated as people. They were exams. Do this gallbladder in this room, do this hip nailing in that room. I was reminded they’re people. They could be my family. They could be my children. That’s why I’m passionate about making sure the technology works and doesn’t get in the way.
Have we reached the pinnacle? No. Is it better? I think it is. But we’re still trying to figure it out every day. As long as we have great people passionate about providing outstanding care and we understand where that ability comes from, we’ll keep moving forward.
We’re a Catholic healthcare system, and our rule is we start most meetings with prayer. We are called to love one another as God loves us, and we need to remember that every day. That’s why I keep doing what I’m doing.
Rohit: Awesome.
Ritu: Thank you so much, Chuck.
Rohit: Really appreciate it.
Charles: Okay. Thanks for the opportunity to share.
————
Subscribe to our podcast series at www.thebigunlock.com and write us at [email protected]
Disclaimer: This Q&A has been derived from the podcast transcript and has been edited for readability and clarity.
About the Hosts
Rohit Mahajan is an entrepreneur and a leader in the information technology and software industry. His focus lies in the field of artificial intelligence and digital transformation. He has also written a book on Quantum Care, A Deep Dive into AI for Health Delivery and Research that has been published and has been trending #1 in several categories on Amazon.
Rohit is skilled in business and IT strategy, M&A, Sales & Marketing and Global Delivery. He holds a bachelor’s degree in Electronics and Communications Engineering, is a Wharton School Fellow and a graduate from the Harvard Business School.
Rohit is the CEO of Damo, Managing Partner and CEO of BigRio, the President at Citadel Discovery, Advisor at CarTwin, Managing Partner at C2R Tech, and Founder at BetterLungs. He has previously also worked with IBM and Wipro. He completed his executive education programs in AI in Business and Healthcare from MIT Sloan, MIT CSAIL and Harvard School of Public Health. He has completed the Global Healthcare Leaders Program from Harvard Medical School.

Ritu M. Uberoy has over twenty-five years of experience in the software and information technology industry in the United States and in India. She established Saviance Technologies in India and has been involved in the delivery of several successful software projects and products to clients in various industry segments.
Ritu completed AI for Health Care: Concepts and Applications from the Harvard T.H. Chan School of Public Health and Applied Generative AI for Digital Transformation from MIT Professional Education. She has successfully taught Gen AI concepts in a classroom setting in Houston and in workshop settings to C-Suite leaders in Boston and Cleveland. She attended HIMSS in March 2024 at Orlando and the Imagination in Action AI Summit at MIT in April 2024. She is also responsible for the GenAI Center of Excellence at BigRio and DigiMTM Digital Maturity Model and Assessment at Damo.
Ritu earned her Bachelor’s degree in Computer Science from Delhi Institute of Technology (now NSIT) and a Master’s degree in Computer Science from Santa Clara University in California. She has participated in the Fellow’s program at The Wharton School, University of Pennsylvania.
About the Legend
Paddy was the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy was also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He was the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He was widely published and had a by-lined column in CIO Magazine and other respected industry publications.