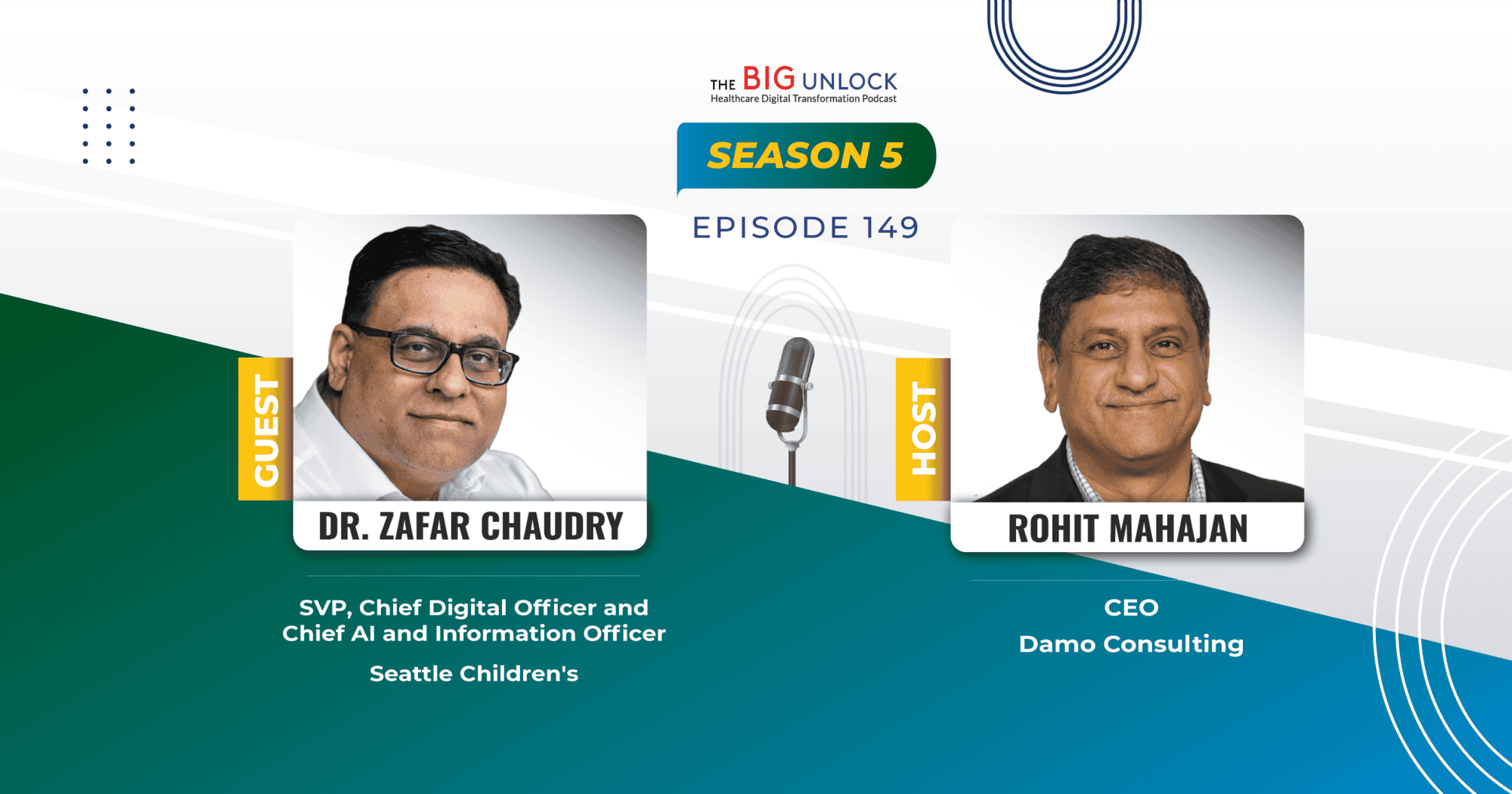
Season 5: Episode #149
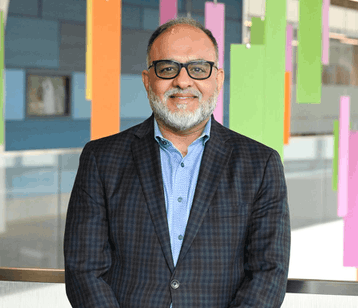
Podcast with Dr. Zafar Chaudry, SVP, Chief Digital Officer and Chief AI and Information Officer, Seattle Children's
AI is Easy to Launch, Hard to Sustain – Focus on People, Processes, and Change Management
Share
In this episode, Dr. Zafar Chaudry, SVP, Chief Digital Officer and Chief AI and Information Officer of Seattle Children’s shares his journey into healthcare and explores the use of AI in transforming the healthcare environment. He discusses innovative use cases, such as developing clinical pathways that are queryable with AI, and a language translation model for discharge instructions to improve patient outcomes. He emphasizes the importance of stakeholder engagement and change management in innovation.
Dr. Chaudry explains their strategic approach to allocating funds, focusing on patient safety, experience, and quality, supported by a prioritization matrix and stakeholder collaboration. He delves into their AI initiatives, including mandatory training, a board-ratified AI policy, and an AI review board to assess projects. He also discusses the evolution of AI technologies, from automation to Generative AI, and stresses the need for robust data protection.
Dr. Chaudry also advises startups to focus on real use cases, building partnerships, and understanding the long-term nature of healthcare. He underscores the value of patience, careful investment, and overcoming resistance to change when implementing AI solutions. Take a listen.
Show Notes |
||||
| 01:14 | What interests you in the healthcare industry segment to become the CIO of a hospital system? | |||
| 02:47 | How long have you been in the leadership position at UMC, where is it located, and what kind of population does it serve? | |||
| 03:35 | You have done a lot of work from technology perspective to support the business needs of the hospital. You've done over 200 applications and transformed the EMR system. Would you like to share with the audience the thought process that drove those changes and what were some of those changes? | |||
| 07:47 | What do you think about your digital transformation efforts? If you could describe a few of them which have had impact on the patient population. | |||
| 08:30 | Please describe in your own, you know, way that what is digital transformation for provider systems such as yours? Where do you see it going? Some of the challenges that you might have faced and how did it actually end up impacting patients? | |||
| 11:24 | How did you manage to change the mindset of the people? How did they manage to change themselves? To adapt to this new world where technology, especially with AI and GenAI and other new technologies which are coming our way, how do you change mindsets and change behaviors and change culture over there? | |||
| 13:00 | Would you like to provide one example of how the technologies which you were implementing, and you continue to be implementing in your hospital system are accessible and usable by a variety of users, including within the hospital and outside the hospital. | |||
| 16:28 | How do you innovate? Do you involve external parties? Do you have some kind of a, you know, innovation focus department? Or is it part and parcel of everybody's, you know, kind of like daily life? | |||
| 19:24 | What are your thoughts on new technologies, especially Gen AI? Have you been experimenting with any predictive analytics or large language models? What would be your advice or thoughts to any other healthcare leaders on how to go about this journey of exploration? | |||
| 22:15 | Standing here now and looking back, if you were able to go back and change one or two things, what would you like to do differently or have done differently? | |||
Video Podcast and Extracts
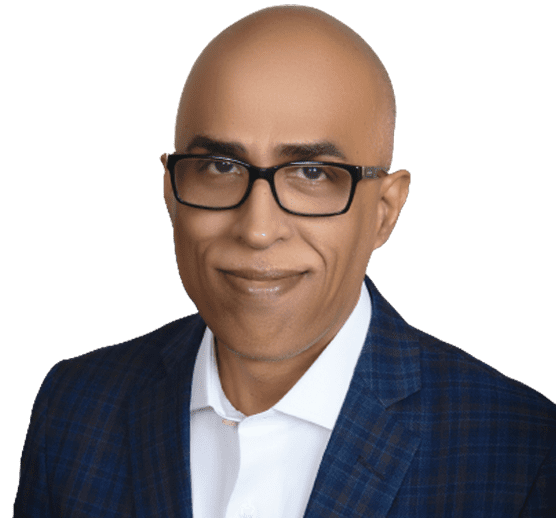
About our guest

Dr. Zafar Chaudry has been Chief Information Officer and Senior Vice President of Seattle Children's since November 06, 2017. He was promoted to Chief Digital Officer and Chief Information Officer in 2021. Through his role, he provides vision and leadership for the development of technology initiatives and enterprise-wide information systems and services for Seattle Children’s. His goal is to enable clinicians with the best technology to deliver safe and excellent care to our patients.
Dr. Chaudry was recently awarded the 2022 CHIME Transformational Leader Award and the 2022 Seattle CIO of the Year ORBIE Awards for Healthcare. He was nominated for the 2021 CHIME - AHA Transformational Leadership Award. He has also been a finalist for the Seattle CIO of the Year ORBIE Awards (2020 and 2021). He is also a member of the global elite list Constellation’s Business Transformation 150 (BT150) 2020; that recognizes the top global executives leading business transformation efforts in their organizations. Dr. Chaudry was named to the Becker’s Hospital Review’s 102 Hospital CIOs to Know (2021), Becker’s Hospital Review’s 100 Hospital CIOs to Know (2019 and 2020), CIO magazine’s list of U.K. CIO’s to follow on Twitter (2019) and Becker's Hospital Review (USA) 105 Hospital and Health System CIOs to Know (2018). He was also named to the CIO.CO.UK’s Top 100 list of the most transformative CIOs in the U.K. (2017) and Government Computing’s top 100 influential technology leaders in the U.K. public sector (2010).
Dr. Chaudry, who began his career as a physician, has more than 30 years of experience in all aspects of information technology. His background includes work in both healthcare and corporate settings in the U.S., Australia, Western Europe, and the U.K., in enterprise infrastructure development; business intelligence; unified telecommunications; and implementation of health care information and electronic medical record systems. He previously served as Chief Information Officer at Cambridge University Hospitals in the United Kingdom. Prior to Cambridge University Hospitals, he served as Global Research Director at Gartner. He also served as Chief Information Officer at the Liverpool Women's and Alder Hey Children's Hospitals in the U.K.; Consulting Editor for Hospital Information Technology Europe Magazine; Information Technology Strategist for the Vision4Children Pediatric Charity in the U.K. and Teaching Faculty at the City Colleges of Chicago.
Dr. Chaudry earned his Doctor of Medicine degree from Ross University. He subsequently earned his Master of Science degree in health care policy and management from the University of Birmingham. He also holds a Master of Science degree in information systems management from the University of Salford and his Master of Business Administration from Aston University, all in the U.K.
Recent Episodes
Q. Please talk about a little bit about your business and your journey in the healthcare sector.
Zafar: Thank you for having me. Pleasure to be here. I am Zafar Chaudry, I’m the Chief Digital AI and Information Officer at Seattle Children’s. I have been here for seven years. Seattle Children’s is a pediatric health system in the Pacific Northwest in the United States. We have 47 sites in Washington, Alaska, Montana, Idaho.
In terms of my journey to where I’m at now, it’s been a very convoluted one. So, I’m a recovering physician. I started my career as a doctor. A doc practiced for a X number of years and then very quickly defected to the dark side. Joined technology in the early 90s when clinical people weren’t necessarily doing IT stuff and I thought this might be a good idea and then went through that journey, did some dot com before it went dot bomb and then leadership roles in health IT and I’ve had many over the last 38 years, uh, in different parts of the world, UK, US, Middle East, Asia pack.
So I’ve, I’ve seen a lot of healthcare delivered in different ways. And I work now in pediatrics because I have worked in pediatrics prior to this. And I like working in pediatrics because There isn’t a day you come to work where you have to think about why you do this job because protecting kids and helping them get healthy is an easy job to do.
So that’s why I’ve been here such a long time, hope to continue the good work. So that’s sort of my very quick high level on how I got here.
Q. So Zafar, tell us more about how do you think about innovation at your system and how do you involve other stakeholders and people in that journey?
Zafar: Innovation is always an interesting one, right? Because I always say to people that first thing you have to do in any healthcare environment is make sure that the basics work really well.
Because doctors, nurses, allied health professionals, patients, parents want your basics to be good. Your infrastructure has to be solid, your end user compute experience has to be solid. So it’s a parallel journey. So you do the, what I like to call the lights on, doors open very well, focus on that. The innovation piece comes in parallel from what you learn in that journey. So a lot of times you can take what you learn from the basics and then figure out, well, how do I make this better? How do I automate? How do I apply technologies that would change the way in which we do things? At Children’s, our digital strategy isn’t a strategy that I come up with.
I have a group of parents and patients. We meet every month and they tell me. What we should build, why we should build it, what they need, because fundamentally, when you’re doing innovation and new developments, you can’t do those in isolation. You have to have stakeholder engagement. So whether you’re talking to a group of doctors about what is a problem they need solving to patients who tell you, They need a way to find locations in your facility.
Those ideas then come together for you to decide what your next level of innovation is going to be. Right. Whether it’s building an app, whether it’s using an automation tool, or whether it’s using, you know, the dreaded AI, which everybody talks about. Of course, of course. Those are all things that you have to figure out.
Yeah, by listening, learning, teaching and collaborating, and that’s what we do very well.
Q. That’s great to know. This is very interesting that you have a group of parents and even, you know, patients. meeting frequently to kind of brainstorm on what the changes or the ideas might be. So Zafar, would you like to talk about anyone or one in particular, let’s say that you think was a good example of such an innovation project?
Zafar: So I’ll give you a very good example. So in one of the discussions two years ago, actually, one of the patients, and what’s interesting about kids. Is the average 12 year old kid is a lot smarter than me when it comes to IT, right? They understand it. They grew up in it. I was having a conversation with a group in that group and the conversation came around.
One of the kids said to me, well, he didn’t think we were doing a very good job because when he’s here for a really long period of time, there’s nothing to keep him engaged, right? And I said, well, that’s true. Okay, so what do you need? And his idea was pediatric hospitals should have a form of gaming to keep kids engaged.
And so from that simple idea, yeah. We are the world’s first organization to have our own Minecraft server, and we built our entire hospital in Minecraft. And we just launched that eight weeks ago on Twitch. So you can come to our hospital as a child, you can become a character in our Minefield Minecraft experience.
And you can do everything that you can do in Minecraft, and we partnered with Microsoft and others to make that happen. And that’s all live. So that’s an example of innovation that I didn’t come up with. Yeah. A child suggested. Yes. We took the idea and we built upon it. I made something amazing. And you actually can see this whole launch on YouTube.
You’ll be able to see it. So that’s awesome. That’s to me is real innovation. Don’t come up with an idea yourself and think it’s amazing. Let somebody tell you what you need. And because it took us about two years to build it and get it ready. Lots of kids have been involved in helping us design, build, test.
Oh, and I’m not a gamer because I’m old, but I can tell you that when I play Minecraft with the kids on launch, you know, I was killed in seconds to do this stuff, right? But they know it. I mean, they live and breathe it. They’re building things down. So I think that’s how you innovate. You find out what people really are passionate about.
And Put some really smart people together, figure out whether that has real value. Now, of course, when I go and now talk to parents and patients about this innovation, we’re getting huge amounts of positive feedback, right? I talked to parents who kids have had serious surgeries who are telling me that by using this environment, their kid was able to manage through the pain, right?
That’s huge. That’s huge. Absolutely. And gaming therapy is the whole area. So my eyes were open to that. We jumped on it. So that’s just one example of how stakeholder engagement. Yeah. Get you to an idea. You can get you to something workable, but you can pass through to a go live. That’s hugely successful.
Q. That’s awesome. That’s awesome. What I’m also curious to learn from you Zafar is that when these ideas bubble up and you know that you have to spend basically time, resources, money behind these initiatives to make them successful, how do you filter or how do you allocate the funds?
Zafar: So we obviously nobody has unlimited funds including us. You do have to do a prioritization exercise, right? But when you’re looking at prioritization and how you allocate funds, you look at key things. Does it affect patient safety? Does it improve patient experience? Is it a quality issue? Is it just an operational issue that needs to be solved? So you set up a set of criteria, but you don’t use those criteria against the list of priorities by yourself in isolation, that’s also a stakeholder engagement process.
So we have to include our clinical teams and our non clinical teams and ask them, would they rank these things higher? In terms of this gaming initiative, for instance, this was kind of different. We do assign some funds to what I describe as RD. So because it was something that hadn’t been done before. I didn’t know if it would actually work, but that fell under experimental R& D.
And I do allocate some funds every year for experimental, because I think it’s very important to be agile and it’s very important to be able to do something well or fail fast. And learn from that and then improve. So this type of project would have fell into that category. Other basic projects would fall into the bigger prioritization matrix, patient safety, all of those things.
And then based on the money you have, you get your list and then there’s a cutoff point, right? So if you have a list, if I look at AI as an example, we have a list of 300 things that people want to do with AI. And we only have funding for maybe the top three. So we had to do a big prioritization piece of work to make that viable.
And then we’d pick the top three items. to fund and test in that sort of particular process when it comes to AI initiatives as an example.
Q. That’s great. So talking about AI, uh, Zafar, I know that you have probably been on the AI journey for some time now. And of course, the Gen AI wave is coming at us fast and furious. Things are changing at a very, uh, So walk us through how you’re dealing with this change and how you have kind of set up the infrastructure for success.
Zafar: So everybody has to look at AI. It’s not going away. So you have to put some focus on it. The way we looked at it was the first thing in any step is to educate people.
So we have made AI training mandatory. So every year there is a module that you have to take that explains AI to you. It’s pros, it’s cons. It’s pitfalls and people then take a test and they pass the test and then they, that’s their mandatory training for the year. In addition, we’ve put together an AI policy that has been ratified by the board.
So everybody knows what the do’s and don’ts are of this technology. Third step is we have an AI review board that has multiple stakeholders from different domains. And that panel meets to review any AI request that comes in. Not only for funding, but it also reviews it for safety. It reviews it for the technology that somebody wants to use to make sure it’s safe to make sure that data is not lost in any way.
Yes. And AI is an evolution, I think, not a revolution. I think we’ve been using AI, most people have for a long time. It’s gone from automation processes to, you know, You have a small data language model that you’ve applied algorithms to, and now as you get to Gen AI. You have a much larger language model, a much larger database, and therefore, the bigger the data feed, the better the outcome will be.
And so we’ve evolved through all of those stages. And yes, we’re now looking at, you know, what does gen AI, we have lots of access to more data points. But you have to protect the data, you have to do all these things, you have to make sure nothing gets out. So that’s the review board’s process. If it’s approved, then we will build it or partner.
To build it to get to prototype because I think with every AI you have to prototype and then you have to test heavily. So to give examples, Seattle Children’s is very well known. You know, we’ve been a top 10 Children’s Hospital for 30 plus years and we’re very well known for our clinical standard pathways of treating certain conditions with kids and we’ve documented all those pathways and over time those pathways are now disseminated to different organizations even across the world and they use them as the standard way to treat conditions. The problem is, you know, It’s hundreds and hundreds, hundreds of PDFs.
Yes. So the old way of looking at how to treat a patient using a standard pathway was to A, find the relevant PDF, then read it, and then figure out what are you going to do. Right. Really long winded process. So we decided, well, how can you make this, uh, a process where you can just use natural language and ask the question, how should I treat a patient with these symptoms and see if we could get the answer.
So we did, we took all of our material and we put it into the AI and the AI obviously read it and tried to understand it. Then we put a series of clinicians To test it. And so now we’re at a point where you can actually ask the A. I. The question. I have a kid with cough with these symptoms. What should the treatment protocol be?
And it will find the answer. It will tell you what to do, and it will reference it back to the document. So it’s instantaneous, right? It’s not, look at me, I’ll come back to this in 30 minutes after I read a whole bunch of documents, right? And it’s evidence based because it’s only based on our evidence, which is all validated evidence.
So we’re in beta phase and it’s working very well. We’ve had 15 teams of people look at this and that’s going to revolutionize how quickly care can be provided. It’s also revolutionary for training new docs because they’re learning and they want to ask a lot of questions so they can learn about different conditions and how to treat them.
It will avoid them reading thousands of pages of documents. But just going to what they need to know, so that’s just one example of how you can, but that was through the review board, built a prototype model, and that’s with Google on Gemini, and then we are testing it once it’s finalized and baked to be safe.
Yeah, it will launch it for all of our clinicians. And that will be a huge win because it will give us speed of treatment whilst it’s still safe, right? Of course. Those are all the keys of biggest worry you have in May Isaac to hallucinate. Yeah. But in this scenario, because the language that you’re feeding into it, the data is restricted to our validated data only. Yes. It has less likelihood to hallucinate because it’s pointing back to the reference document.
Q. Great. Yeah. That is, I think the way to go. In fact, at BigRio, we have an accelerator of which does such a thing using, I’m using a technical term here, Zafar, but I think in the audience, many people know this already, the RAG techniques.
So this is a fantastic use case that you have there, you know, congratulations on this one. So Zafar share with us any other. Key initiatives on AI or Gen AI that either you might be looking at in the near future or you think other healthcare organizations might benefit from if you’re looking in the crystal ball, you know, in the near future, short term and long term future. What do you see?
Zafar: I think in this particular model of Gen AI, the sky’s the limit. So for us, the next thing we’re testing already is. How do you, so when a patient comes, we send the patient home, we give them discharge instructions. This is how you’re supposed to take care of yourself after you leave. The challenge is in a multicultural society, not everybody is, primary language is English and what we found here in Seattle is.
Yes, English is predominant, but so is Spanish, so is Somali, so is Ukrainian. So we were still giving people discharge instructions in English. So we’ve done the same thing. We’ve built a model in AI that can take these instructions, accurately translate them into the language that you want, and then we’re able to give the patient the right instructions in the right language.
That will be a huge win because many patients aren’t primarily English speaking. Yes, it seems like a simple use case, but we were failing because we were giving people instructions in English. They weren’t following the instructions. The problem is if you don’t follow the instructions, there’s a high likelihood that within the first 30 days, you’ll come back and come back.
You could be readmitted. That’s not a good outcome. It’s not safe. So we’ve done that same process design prototype test. It’s in beta, and it’s working very well. And once we fully tested it, that’s another one that we could launch. And actually, that’s not even a specific use case for us. Anybody Yeah, could do that because we are unique in the fact that we are treating patients who have multiple languages, right?
Every region in the country has that. So that’s just another way of looking at it. But these are all prioritized things. Everything, of course, in AI is limited by the cash that you have. Yeah, some initiatives. Can be inexpensive, but many are very expensive to launch more of an invest to save scheme. Yes, can’t immediately get gratification and savings and AI, although many people tried to tell you that’s the case.
It’s not the case. That’s true. But you have to be very careful in what you invest in and then you see what that return could be over a period of time. So you need, you need a lot of patience. Yes. Obviously some tech companies will want to tell you that launch this and immediately you will see benefits.
You don’t always immediately get the cash benefits you need to pay for ongoing. So what I like to say to people is AI is definitely the way forwards. It is. Revolutionary and how it will assist people to work in health care in the future and scale faster our services in health care, but it is easy to launch is very hard to sustain. And that’s the big takeaway for me is I can do 15 more AI launches. Right. Within weeks, but they won’t sustain because what everybody fails to remember in any technology world, it’s about the people and process and change management is really important. The key actually. You can’t have an AI because think about the fear of it.
So I want to do an AI that translates discharge instructions. I think it’s a good idea. We’ve tested it. It’s a good idea. But the change management for that is assuring the people that we have that somehow it’s not just going to take your job. So even though we will give you a printout if that’s what you want in the language of your choice, that doesn’t take away from the nurse Who still needs to tell the parents and the kid what they need to do to take care of themselves at home.
Exactly. It’s not that we’ll miss that step altogether and just hand you this paper and say, good luck. Of course. But people immediately think, Oh my God, my job’s going away. My job is going to be minimalized and they’re going to reduce all these people. But we wouldn’t do that because in nursing, for example, we have a shortage.
Yeah. So to actually allow nurses to do their job and not be as stressed. Burnout is real, right? In the clinical side of medicine, then these tools, you still have to educate the user on why this tool is good for you and how you can sustain it versus, oh, here’s just another great tech idea. Of course, of course.
Q. So one thing which I would like to touch upon before we wrap up Zafar is around the idea of what would be your suggestions and advice for startups in healthcare. There are so many startups, some well funded, some less funded at various stages from seed to series E sometimes. There’s so many. So many. So what would you say to someone who was wanting to do startups in healthcare?
Zafar: So my best advice is, is that if you want to understand how healthcare functions, there’s a couple of points. One is, healthcare is the long game. It’s not the short game. If you build a startup in healthcare, You really need to be ready to go the distance. This is not instant gratification. The margins in healthcare IT are much lower.
So if you build an AI startup in healthcare, A, it’s going to take you some years to build traction. So you’re going to have to have funding to do that. B, If you think you’re going to make triple and double digit margins from a health system, you’re fooling yourself because you’re not. It’s always single digit margins.
The benefit in healthcare though, is once you do good work and you have a relationship, you will get those single digit margins for a really, really long time. It’s a relationship business, right? Yes. So if you’re one of those entrepreneurs who says, I just want to build the next company and cash out, I wouldn’t recommend health it based companies because they don’t happen that quickly.
If you tend to follow that model, they flame out. I would certainly, certainly say that. The other thing I would advise startups is if you’re in this new space of AI. And you really want to make an impact and build partnerships and get the logos you need to grow your business, build real use cases that people can test.
Yes, don’t come in and say you can deliver the world if somebody pays you a whole bunch of professional services, because that’s too risky for people like me. But if you came to me and said, I actually have built five use cases. That we’ve tested with sample data, but we would like you to try with your data, then I would probably try it.
What I don’t want to be is be a software development house, right? I don’t want to spend a year and a million dollars in professional services building an AI model that actually ends up failing. Because that’s not a good use of our money. Our money traditionally should go into getting patients better.
Yes. And healthy, not, of course, we did a partnership with you. We lost 500 K and didn’t get any output. So if you are brand new and you’re funded, build three good use cases. How would you build those use cases? Make sure you have an advisory group of clinical people, people with healthcare backgrounds who can guide you on how to build those use cases three use cases, then bring those use cases to your sales cycle, and you’ll have more success.
That’s awesome advice, Zafar. And with that, I would like to thank you for sparing your time for this podcast. Really appreciate it.
Thanks for having me.
We hope you enjoyed this podcast. Subscribe to our podcast series at www.thebigunlock.com and write to us at [email protected]
Disclaimer: This Q&A has been derived from the podcast transcript and has been edited for readability and clarity.
About the host
Paddy is the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy is also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He is the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He is widely published and has a by-lined column in CIO Magazine and other respected industry publications.
About the Host

Ritu M. Uberoy has over twenty-five years of experience in the software and information technology industry in the United States and in India. She established Saviance Technologies in India and has been involved in the delivery of several successful software projects and products to clients in various industry segments.
Ritu completed AI for Health Care: Concepts and Applications from the Harvard T.H. Chan School of Public Health and Applied Generative AI for Digital Transformation from MIT Professional Education. She has successfully taught Gen AI concepts in a classroom setting in Houston and in workshop settings to C-Suite leaders in Boston and Cleveland. She attended HIMSS in March 2024 at Orlando and the Imagination in Action AI Summit at MIT in April 2024. She is also responsible for the GenAI Center of Excellence at BigRio and DigiMTM Digital Maturity Model and Assessment at Damo.
Ritu earned her Bachelor’s degree in Computer Science from Delhi Institute of Technology (now NSIT) and a Master’s degree in Computer Science from Santa Clara University in California. She has participated in the Fellow’s program at The Wharton School, University of Pennsylvania.
About the Host
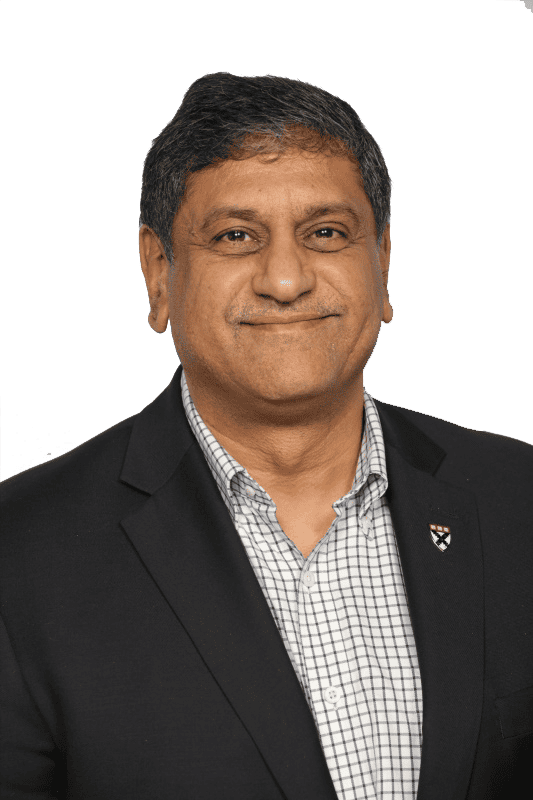
Rohit Mahajan is an entrepreneur and a leader in the information technology and software industry. His focus lies in the field of artificial intelligence and digital transformation. He has also written a book on Quantum Care, A Deep Dive into AI for Health Delivery and Research that has been published and has been trending #1 in several categories on Amazon.
Rohit is skilled in business and IT strategy, M&A, Sales & Marketing and Global Delivery. He holds a bachelor’s degree in Electronics and Communications Engineering, is a Wharton School Fellow and a graduate from the Harvard Business School.
Rohit is the CEO of Damo, Managing Partner and CEO of BigRio, the President at Citadel Discovery, Advisor at CarTwin, Managing Partner at C2R Tech, and Founder at BetterLungs. He has previously also worked with IBM and Wipro. He completed his executive education programs in AI in Business and Healthcare from MIT Sloan, MIT CSAIL and Harvard School of Public Health. He has completed the Global Healthcare Leaders Program from Harvard Medical School.
About the Legend
Paddy was the co-author of Healthcare Digital Transformation – How Consumerism, Technology and Pandemic are Accelerating the Future (Taylor & Francis, Aug 2020), along with Edward W. Marx. Paddy was also the author of the best-selling book The Big Unlock – Harnessing Data and Growing Digital Health Businesses in a Value-based Care Era (Archway Publishing, 2017). He was the host of the highly subscribed The Big Unlock podcast on digital transformation in healthcare featuring C-level executives from the healthcare and technology sectors. He was widely published and had a by-lined column in CIO Magazine and other respected industry publications.









 Hosted by Rohit Mahajan
Hosted by Rohit Mahajan